Perinatal asphyxia
| Perinatal asphyxia | |
|---|---|
| Classification and external resources | |
| Specialty | pediatrics |
| ICD-10 | P21 |
| ICD-9-CM | 768 |
| DiseasesDB | 1416 |
| eMedicine | ped/149 |
| MeSH | D001238 |
Perinatal asphyxia, neonatal asphyxia or birth asphyxia is the medical condition resulting from deprivation of oxygen to a newborn infant that lasts long enough during the birth process to cause physical harm, usually to the brain. Hypoxic damage can occur to most of the infant's organs (heart, lungs, liver, gut, kidneys), but brain damage is of most concern and perhaps the least likely to quickly or completely heal. In more pronounced cases, an infant will survive, but with damage to the brain manifested as either mental, such as developmental delay or intellectual disability, or physical, such as spasticity.
It results most commonly from a drop in maternal blood pressure or some other substantial interference with blood flow to the infant's brain during delivery. This can occur due to inadequate circulation or perfusion, impaired respiratory effort, or inadequate ventilation. Perinatal asphyxia happens in 2 to 10 per 1000 newborns that are born at term, and more for those that are born prematurely.[1] WHO estimates that 4 million neonatal deaths occur yearly due to birth asphyxia, representing 38% of deaths of children under 5 years of age.[2]
An infant suffering severe perinatal asphyxia usually has poor color (cyanosis), perfusion, responsiveness, muscle tone, and respiratory effort, as reflected in a low 5 minute Apgar score. Extreme degrees of asphyxia can cause cardiac arrest and death. If resuscitation is successful, the infant is usually transferred to a neonatal intensive care unit.
There has long been a scientific debate over whether newborn infants with asphyxia should be resuscitated with 100% oxygen or normal air.[3] It has been demonstrated that high concentrations of oxygen lead to generation of oxygen free radicals, which have a role in reperfusion injury after asphyxia.[4] Research by Ola Didrik Saugstad and others led to new international guidelines on newborn resuscitation in 2010, recommending the use of normal air instead of 100% oxygen.[5][6]
There is considerable controversy over the diagnosis of birth asphyxia due to medicolegal reasons.[7][8] Because of its lack of precision, the term is eschewed in modern obstetrics.[9]
Risk Factors
- Increasing or decreasing maternal age
- Prolonged rupture of membranes
- Meconium-stained fluid
- Multiple births
- Lack of antenatal care
- Low birth weight infants
- Malpresentation
- Augmentation of labour with oxytocin
- Antepartum hemorrhage
- Severe eclampsia and pre-eclampsia
- Antepartum and intrapartum anemia[10]
Cause
- Inadequate oxygenation of maternal blood due to hypoventilation during anesthesia, heart diseases, pneumonia, respiratory failure
- Low maternal blood pressure due to hypotension e.g. compression of vena cava and aorta, excess anaesthesia
- Inadequate relaxation of uterus due to excess oxytocin
- Premature separation of placenta
- Placental insufficiency
- Knotting of umbilical cord around the neck of infant
Treatment
- A= Establish open airway: Suctioning, if necessary endotracheal intubation
- B= Breathing: Through tactile stimulation, PPV, bag and mask, or through endotracheal tube
- C= Circulation: Through chest compressions and dedications if needed
- D= Drugs: Adrenaline .01 of .1 solution
- Hypothermia treatment to reduce the extent of brain injury
Epinephrine .01 dose 10
Saline solution for hypovolemia
Epidemiology
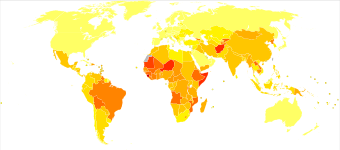
A 2008 bulletin from the World Health Organization estimates that 900,001 total infants die each year from birth asphyxia, making it a leading cause of death for newborns.[11]
In the United States, intrauterine hypoxia and birth asphyxia was listed as the tenth leading cause of neonatal death.[12]
Medicolegal Aspects
There is current controversy regarding the medicolegal definitions and impacts of birth asphyxia. Plaintiff's attorneys often take the position that birth asphyxia is often preventable, and is often due to substandard care and human error.[13] They have utilized some studies in their favor that have demonstrated that, "...although other potential causes exist, asphyxia and hypoxic-ischemic encephalopathy affect a substantial number of babies, and they are preventable causes of cerebral palsy."[14][15][16] The American Congress of Obstetricians and Gynecologists disputes that conditions such as cerebral palsy are usually attributable to preventable causes, instead associating them with circumstances arising prior to birth and delivery.[17]
References
- ↑ "Brain damage from perinatal asphyxia: correlation of MR findings with gestational age -- Barkovich and Truwit 11 (6): 1087 -- American Journal of Neuroradiology". www.ajnr.org. Retrieved 2008-03-27.
- ↑ Aslam, Hafiz Muhammad; Saleem, Shafaq; Afzal, Rafia; Iqbal, Umair; Saleem, Sehrish Muhammad; Shaikh, Muhammad Waqas Abid; Shahid, Nazish (2014-12-20). "Risk factors of birth asphyxia". Italian Journal of Pediatrics. 40. doi:10.1186/s13052-014-0094-2. ISSN 1824-7288. PMC 4300075
 . PMID 25526846.
. PMID 25526846. - ↑ Davis, PG; Tan, A; O'Donnell, CPF; Schulze, A (2004). "Resuscitation of newborn infants with 100% oxygen or air: a systematic review and meta-analysis". The Lancet. 364: 1329–1333. doi:10.1016/S0140-6736(04)17189-4. PMID 15474135.
- ↑ Kutzsche, S; Ilves, P; Kirkeby, OJ; Saugstad, OD (2001). "Hydrogen peroxide production in leukocytes during cerebral hypoxia and reoxygenation with 100% or 21% oxygen in newborn piglets". Pediatric Research. 49: 834–842. doi:10.1203/00006450-200106000-00020. PMID 11385146.
- ↑ ILCOR Neonatal Resuscitation Guidelines 2010
- ↑ Norwegian paediatrician honoured by University of Athens, Norway.gr
- ↑ Blumenthal, I (2001). "Cerebral palsy—medicolegal aspects". Journal of the Royal Society of Medicine. 94 (12): 624–7. PMC 1282294
 . PMID 11733588.
. PMID 11733588. - ↑ Dhar, KK; Ray, SN; Dhall, GI (1995). "Significance of nuchal cord". Journal of the Indian Medical Association. 93 (12): 451–3. PMID 8773129.
- ↑ ACOG. "Committee Opinion, Number 326, December 2005: Inappropriate Use of the Terms Fetal Distress and Birth Asphyxia". Retrieved June 9, 2010.
- ↑ Kaye, D. (2003-03-01). "Antenatal and intrapartum risk factors for birth asphyxia among emergency obstetric referrals in Mulago Hospital, Kampala, Uganda". East African Medical Journal. 80 (3): 140–143. doi:10.4314/eamj.v80i3.8683. ISSN 0012-835X. PMID 12762429.
- ↑ Spector J, Daga S. "Preventing those so-called stillbirths". WHO. Retrieved 13 December 2013.
- ↑ National Center for Health Statistics
- ↑ Andreasen, Stine. "Acta Obstetricia et Gynecologica". Wiley Online Library. Retrieved April 8, 2016.
- ↑ "APFEL Handout: Birth Asphyxia & Cerebral Palsy" (PDF). Colorado Bar Association. Retrieved April 8, 2016.
- ↑ Cohen, Frances M. (2003). "Origin and Timing of Brain Lesions in Term Infants with Neonatal Encephalopathy". The Lancet. PMID 12620738.
- ↑ Becher, J-C; Stenson, Bj; Lyon, Aj (2007-11-01). "Is intrapartum asphyxia preventable?". BJOG: An International Journal of Obstetrics & Gynaecology. 114 (11): 1442–1444. doi:10.1111/j.1471-0528.2007.01487.x. ISSN 1471-0528.
- ↑ Van Eerden, Peter. "Summary of the Publication, "Neonatal Encephalopathy and Cerebral Palsy: Defining the Pathogenesis and Pathophysiology," by the ACOG Task Force on Neonatal Encephalopathy and Cerebral Palsy". Medscape. Retrieved April 8, 2016.
External links
- Asphyxia neonatorum, School of Child and Adolescent Health, University of Cape Town