Sensory processing disorder
| Sensory processing disorder | |
|---|---|
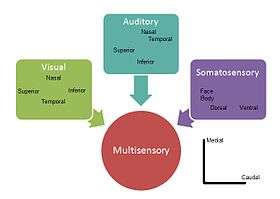 Example of how visual, auditory and somatosensory information merge into multisensory integration representation in the superior colliculus | |
| Pseudomedical diagnosis | |
| Risks | Nocebo |
Sensory processing disorder (SPD; also known as sensory integration dysfunction) is a controversial condition that exists when multisensory integration is not adequately processed in order to provide appropriate responses to the demands of the environment.
The senses provide information from various modalities—vision, audition, tactile, olfactory, taste, proprioception, and vestibular system—that humans need to function. Sensory processing disorder is characterized by significant problems to organize sensation coming from the body and the environment and manifested by difficulties in the performance in one or more of the main areas of life: productivity, leisure and play[1] or activities of daily living.[2] Different people experience a wide range of difficulties when processing input coming from a variety of senses, particularly tactile (e.g., finding fabrics itchy and hard to wear while others do not), vestibular (e.g., experiencing motion sickness while riding a car) and proprioceptive (having difficulty grading the force to hold a pen in order to write).
Sensory integration was defined by occupational therapist Anna Jean Ayres in 1972 as "the neurological process that organizes sensation from one's own body and from the environment and makes it possible to use the body effectively within the environment".[3][4]
Classification
Sensory processing disorders are classified into three broad categories: sensory modulation disorder, sensory-based motor disorders and sensory discrimination disorders (as defined in the Diagnostic Classification of Mental Health and Developmental Disorders in Infancy and Early Childhood).[5][6][7]
Sensory modulation disorder (SMD)
Sensory modulation refers to a complex central nervous system process[5][8] by which neural messages that convey information about the intensity, frequency, duration, complexity, and novelty of sensory stimuli are adjusted.[9] Those with SMD present difficulties processing the degree of intensity, duration, frequency, etc., of information and may exhibit behaviors with a fearful or anxious pattern, negative or stubborn behaviors, self-absorbed behaviors that are difficult to engage, or creative or actively seeking sensation.[10]
SMD consists of three subtypes:
- Sensory over-responsivity
- Sensory under-responsivity
- Sensory craving/seeking
Sensory-based motor disorder (SBMD)
Sensory-based motor disorder shows motor output that is disorganized as a result of incorrect processing of sensory information affecting postural control challenges, resulting in postural disorder, or developmental coordination disorder.[5][11]
The SBMD subtypes are:
- Dyspraxia
- Postural disorder
Sensory discrimination disorder (SDD)
Sensory discrimination disorder involves the incorrect processing of sensory information.[5] Incorrect processing of visual or auditory input, for example, may be seen in inattentiveness, disorganization, and poor school performance.
The SDD subtypes are:
- Visual
- Auditory
- Tactile
- Taste
- Smell
- Position/movement
- Interoception.
Signs and symptoms
Symptoms may vary according to the disorder's type and subtype present. SPD can affect one sense or multiple senses. While many people can present one or two symptoms, sensory processing disorder has to have a clear functional impact on the person's life.
Signs of over-responsivity
- Dislike of textures such as those found in fabrics, foods, grooming products or other materials found in daily living, to which most people would not react.
- Avoiding crowds and noisy places
- Motion sickness without medical cause
- Refusal of kissing, cuddling or hugging due to negative experience of touch sensation (not to be confused with shyness or social difficulties)
- Serious discomfort, sickness or threat induced by normal sounds, lights, movements, smells, tastes, or even inner sensations such as heartbeat.
- Picky eating
- Sleep disorders (waking up by minor sounds, problems getting sleep because of sensory overload)
- Difficulty with calming self, feeling constantly under stress
Signs of under-responsivity
- Difficulty waking up
- Sluggishness and lack of responsiveness
- Lack of awareness of pain or other people
- Apparent deafness even when auditory function have been tested
- Difficulty with toilet training, lack of awareness of being wet or soiled
Sensory craving
- Fidgeting
- Seeking or making loud, disturbing noises
- Climbing, jumping, and crashing
- Seeking "extreme" sensations
- Sucking or biting fingers, clothing, pencils, etc.
- Impulsiveness
Sensorimotor-based problems
- Slow and uncoordinated movements
- Poor handwriting
- Poor posture
 Poor posture with Anterior pelvic tilt
Poor posture with Anterior pelvic tilt - Delays in crawling, standing, walking or running.
- Verbosity in order to avoid motor tasks
Sensory discrimination problems
- Things constantly dropped
- Difficulty dressing and eating
- Inappropriate force used to handle objects
Other signs and symptoms
- Poorly integrated balance and rightening reflexes
- Low muscle tone patterns in extensor versus gravity and flexor versus gravity muscle systems
- Poor core tone
- Low postural control
- Poor nystagmus
- Presence of non integrated reflexes such as ATNR
- Jerky eye tracking
- Poor tactile astereognosis
- Inadequate motor, ideational or constructional praxis
- Difficulties with planning movement using feedback information
- Difficulties with planning movement using feedforward information
Causes
The mid-brain and brain stem regions of the central nervous system are early centers in the processing pathway for multisensory integration,[12] these brain regions are involved in processes including coordination, attention, arousal, and autonomic function. After sensory information passes through these centers, it is then routed to brain regions responsible for emotions, memory, and higher level cognitive functions. Sensory processing disorder not only affects interpretation and reaction to stimuli at the midbrain areas, but impacts several higher functions. Damage in any part of the brain involved in multisensory processing can cause difficulties to adequately process stimuli in a functional way.
Current research in sensory processing is focused on finding the genetic and neurological causes of SPD. EEG[13] and measuring event-related potential (ERP) are traditionally used to explore the causes behind the behaviors observed in SPD. Some of the proposed underlying causes by current research are:
- Differences in tactile and auditory over responsivity show moderate genetic influences, with tactile over responsivity demonstrating greater heritability. Bivariate genetic analysis suggested different genetic factors for individual differences in auditory and tactile SOR.[14]
- People with Sensory Processing Deficits have less sensory gating (electrophysiology) than typical subjects.[15][16]
- People with sensory over-responsivity might have increased D2 receptor in the striatum, related to aversion to tactile stimuli and reduced habituation. In animal models, prenatal stress significantly increased tactile avoidance.[17]
- Studies using event-related potentials (ERPs) in children with the sensory over responsivity subtype found atypical neural integration of sensory input. Different neural generators could be activated at an earlier stage of sensory information processing in people with SOR than in typically developing individuals. The automatic association of causally related sensory inputs that occurs at this early sensory-perceptual stage may not function properly in children with SOR. One hypothesis is that multisensory stimulation may activate a higher-level system in frontal cortex that involves attention and cognitive processing, rather than the automatic integration of multisensory stimuli observed in typically developing adults in auditory cortex.[18]
- Recent research found an abnormal white matter microstructure in children with SPD, compared with typical children and those with other neurological disorders such as autism and ADHD.[19][20]
Research
A study conducted by UCSF (University of California San Francisco), shows promise into learning more about how and why people are affected by the sensory processing disorder. According to research by the University there is substantial evidence to show the there are quantifiable differences in the brains of people with SPD compared to those who do not have the disorder. In the study, researchers used an advanced form of MRI called diffusion tensor imaging (DTI), this measures microscopic movement of water molecules within the brain in order to give information about the brain’s white matter tracts (Bunim). The study examined a group of 16 boys between the ages of 8 and 11. These children all have SPD but none of the children also have a diagnosis of Autism. The results of the MRI detected abnormal white matter tracts in the SPD children, particularly in areas in the back of the brain. There are areas that serve as connections for the auditory, visual and tactile systems involved in sensory processing, including their connections between the left and right halves of the brain.[21]
Diagnosis
Sensory processing disorder is currently accepted in the Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0-3R) and is not recognized as a mental disorder in medical manuals such as the ICD-10[22] or the DSM-5.[23]
Diagnosis is primarily arrived at by the use of standardized tests, standardized questionnaires, expert observational scales, and free play observation at an occupational therapy gym. Observation of functional activities might be carried at school and home as well. Some scales that are not exclusively used in SPD evaluations are used to measure visual perception, function, neurology and motor skills.[24]
Depending on the country, diagnosis is made by different professionals, such as occupational therapists, psychologists, learning specialists, physiotherapists and/or speech and language therapists.[25] In some countries it is recommended to have a full psychological and neurological evaluation if symptoms are too severe.
Standardized tests
- Sensory Integration and Praxis Test. (SIPT)
- DeGangi-Berk Test of Sensory Integration (TSI)
- Test of Sensory Functions in Infants (TSFI)[26]
Standardized questionnaires
- Sensory Profile, (SP)[27]
- Infant/Toddler Sensory Profile[26]
- Adolescent/Adult Sensory Profile
- Sensory Profile School Companion
- Sensory Processing Measure (SPM)[28]
- Sensory Processing Measure Preeschool (SPM-P)[29]
Other tests
- Clinical Observations of Motor and Postural Skills (COMPS)[30]
- Developmental Test of Visual Perception: Second Edition (DTVP-2)[31]
- Beery–Buktenica Developmental Test of Visual-Motor Integration, 6th Edition (BEERY VMI)
- Miller Function & Participation Scales
- Bruininks–Oseretsky Test of Motor Proficiency, Second Edition (BOT-2)[32]
- Behavior Rating Inventory of Executive Function (BRIEF)[33][34]
Treatment
Several therapies have been developed to treat SPD.
Sensory integration therapy
The main form of sensory integration therapy is a type of occupational therapy that places a child in a room specifically designed to stimulate and challenge all of the senses.
During the session, the therapist works closely with the child to provide a level of sensory stimulation that the child can cope with, and encourage movement within the room. Sensory integration therapy is driven by four main principles:
- Just right challenge (the child must be able to successfully meet the challenges that are presented through playful activities)
- Adaptive response (the child adapts his behavior with new and useful strategies in response to the challenges presented)
- Active engagement (the child will want to participate because the activities are fun)
- Child directed (the child's preferences are used to initiate therapeutic experiences within the session)
Sensory processing therapy
This therapy retains all of the above-mentioned four principles and adds:[35]
- Intensity (person attends therapy daily for a prolonged period of time)
- Developmental approach (therapist adapts to the developmental age of the person, against actual age)
- Test-retest systematic evaluation (all clients are evaluated before and after)
- Process driven vs. activity driven (therapist focuses on the "Just right" emotional connection and the process that reinforces the relationship)
- Parent education (parent education sessions are scheduled into the therapy process)
- "joie de vivre" (happiness of life is therapy's main goal, attained through social participation, self-regulation, and self-esteem)
- Combination of best practice interventions (is often accompanied by integrated listening system therapy, floor time, and electronic media such as Xbox Kinect, Nintendo Wii, Makoto II machine training and others)
Other methods
Some of these treatments (for example, sensorimotor handling) have a questionable rationale and no empirical evidence. Other treatments (for example, prism lenses, physical exercise, and auditory integration training) have had studies with small positive outcomes, but few conclusions can be made about them due to methodological problems with the studies.[36] Although replicable treatments have been described and valid outcome measures are known, gaps exist in knowledge related to sensory integration dysfunction and therapy.[37] Empirical support is limited, therefore systematic evaluation is needed if these interventions are used.[38]
Children with hypo-reactivity may be exposed to strong sensations such as stroking with a brush, vibrations or rubbing. Play may involve a range of materials to stimulate the senses such as play dough or finger painting.
Children with hyper-reactivity may be exposed to peaceful activities including quiet music and gentle rocking in a softly lit room. Treats and rewards may be used to encourage children to tolerate activities they would normally avoid.
While occupational therapists using a sensory integration frame of reference work on increasing a child's ability to adequately process sensory input, other OTs may focus on environmental accommodations that parents and school staff can use to enhance the child's function at home, school, and in the community.[39][40] These may include selecting soft, tag-free clothing, avoiding fluorescent lighting, and providing ear plugs for "emergency" use (such as for fire drills).
Adults
There is a growing evidence base that points to and supports the notion that adults also show signs of sensory processing difficulties. In the United Kingdom early research and improved clinical outcomes for clients assessed as having sensory processing difficulties is indicating that the therapy may be an appropriate treatment.[41] The adult clients show a range of presentations including autism and Asperger's syndrome, as well as developmental coordination disorder and some mental health difficulties.[42] Therapists suggest that these presentations may arise from the difficulties adults with sensory processing difficulties encounter trying to negotiate the challenges and demands of engaging in everyday life.[43] It is important when treating adults not only to focus upon sensory regulation but to also help them develop and maintain social supports.[44] Adults who are sensory over-responsive have very high correlated anxiety and depression levels compared to adults who do not have sensory over-responsiveness. This is correlated to the perceived absence of social supporters.[44] Sensory processing disorder can also be correlated with sleep quality in adults. This correlation can be seen especially in adults who have low neurological thresholds (sensory sensitivity and sensory avoidance). These individuals are more sensitive to tactile, auditory and visual stimuli which often impacts their quality of sleep.[45]
Epidemiology
It is estimated that up to 16.5% of elementary school aged children present elevated SOR behaviors in the tactile or auditory modalities.[46] However, this figure might represent an underestimation of Sensory Over Responsivity prevalence, since this study did not include children with developmental disorders or those delivered preterm, who are more likely to present it.
This figure is, nonetheless, larger than what previous studies with smaller samples had shown: an estimate of 5–13% of elementary school aged children.[47] Incidence for the remaining subtypes is currently unknown.
Relationship to other disorders
Because comorbid conditions are common with sensory integration issues, a person may have other conditions as well. People who receive the diagnosis of sensory processing disorder may also have signs of anxiety problems, ADHD,[48] food intolerances, behavioral disorders and other disorders.
Autistic spectrum disorders and difficulties of sensory processing
Sensory processing disorder is a common comorbidity with autism spectrum disorders[49][50][51][52][53][54][55] and is now included as part of the symptomatology in the DSMV.
The abnormally high synchrony between the sensory cortices involved in perception and subcortical regions relaying information from the sensory organs to the cortex is pointed as having a central role in the hypersensitivity and other sensory symptoms that define autism spectrum disorder.[56] Sensory modulation has been the main subtype studied. Differences are greater for under-responsivity (for example, walking into things) than for over-responsivity (for example, distress from loud noises) or for sensory seeking (for example, rhythmic movements).[57] The responses may be more common in children: a pair of studies found that autistic children had impaired tactile perception while autistic adults did not.[58]
The Sensory Experiences Questionnaire has been developed to help identify the sensory processing patterns of children who may have autism.[59][60]
SPD and ADHD
It is speculated that SPD may be a misdiagnosis for persons with attention problems.[48] For example, a student who fails to repeat what has been said in class (due to boredom or distraction) might be referred for evaluation for sensory integration dysfunction. The student might then be evaluated by an occupational therapist to determine why they are having difficulty focusing and attending, and perhaps also evaluated by an audiologist or a speech-language pathologist for auditory processing issues or language processing issues.[48] Similarly, a child may be mistakenly labeled "Attention deficit hyperactivity disorder (ADHD)" because impulsivity has been observed, when actually this impulsivity is limited to sensory seeking or avoiding.[61][62] A child might regularly jump out of their seat in class despite multiple warnings and threats because their poor proprioception (body awareness) causes them to fall out of their seat, and their anxiety over this potential problem causes them to avoid sitting whenever possible. If the same child is able to remain seated after being given an inflatable bumpy cushion to sit on (which gives them more sensory input), or, is able to remain seated at home or in a particular classroom but not in their main classroom, it is a sign that more evaluation is needed to determine the cause of their impulsivity.
Other comorbidities
Various conditions can involve SPD, such as obsessive compulsive disorder,[63] schizophrenia,[64][65][66] succinic semialdehyde dehydrogenase deficiency,[67] primary nocturnal enuresis,[68] prenatal alcohol exposure, learning difficulties[17] and people with traumatic brain injury[69] or who have had cochlear implants placed.[70] and may have genetic conditions such as fragile X syndrome.
Controversy
Manuals
SPD is in Stanley Greenspan's Diagnostic Manual for Infancy and Early Childhood and as Regulation Disorders of Sensory Processing part of the The Zero to Three's Diagnostic Classification.[71] but is not recognized in the manuals ICD-10 or in the recently updated DSM-5.[72] However, unusual reactivity to sensory input or unusual interest in sensory aspects is included as a possible but not necessary criterion for the diagnosis of autism.[73]
Misdiagnosis
Some state that sensory processing disorder is a distinct diagnosis, while others argue that differences in sensory responsiveness are features of other diagnoses and it is not a standalone diagnose.[74] The American Academy of Pediatrics, for example, advises against a diagnosis of SPD. However difficulty tolerating or processing sensory information is a characteristic that may be seen in many developmental behavioral disorders, including autism spectrum disorder, attention-deficit/hyperactivity disorder, developmental coordination disorder, or childhood anxiety disorder.[75] The neuroscientist David Eagleman has proposed that SPD may be a form of synesthesia, a perceptual condition in which the senses are blended.[76] Specifically, Eagleman suggests that instead of a sensory input "connecting to [a person's] color area [in the brain], it's connecting to an area involving pain or aversion or nausea".[77][78][79]
Researchers have described a treatable inherited sensory overstimulation disorder that meets diagnostic criteria for both attention deficit disorder and sensory integration dysfunction.[80]
Research
Over 130 articles on sensory integration have been published in peer-reviewed (mostly occupational therapy) journals. The difficulties of designing double-blind research studies of sensory integration dysfunction have been addressed by Temple Grandin and others. Because the amount of research regarding the effectiveness of SPD therapy is limited and inconclusive, the American Academy of Pediatrics advises pediatricians to inform families about these limitations, talk with families about a trial period for SPD therapy, and teach families how to evaluate therapy effectiveness.[75]
History
Sensory processing disorders were first described in-depth by occupational therapist Anna Jean Ayres (1920–1989). According to Ayres's writings, an individual with SPD would have a decreased ability to organize sensory information as it comes in through the senses.[81]
Original model
Ayres's theoretical framework for what she called Sensory integration was developed after six factor analytic studies of populations of children with learning disabilities, perceptual motor disabilities and normal developing children.[82] Ayres created the following nosology based on the patterns that appeared on her factor analysis:
- Dyspraxia: poor motor planning (more related to the vestibular system and proprioception)
- Poor bilateral integration: inadequate use of both sides of the body simultaneously
- Tactile defensiveness: negative reaction to tactile stimuli
- Visual perceptual deficits: poor form and space perception and visual motor functions
- Somatodyspraxia: poor motor planning (related to poor information coming from the tactile and proprioceptive systems)
- Auditory-language problems
Both visual perceptual and auditory language deficits were thought to possess a strong cognitive component and a weak relationship to underlying sensory processing deficits, so they are not considered central deficits in many models of sensory processing.
In 1998, Mulligan performed a study on 10,000 sets of data, each representing an individual child. She performed confirmatory and exploratory factor analyses and found similar patterns of deficits with her data as Ayres did.[83]
Quadrant model
Dunn's nosology uses two criteria:[84] response type (passive vs active) and sensory threshold to the stimuli (low or high) creating 4 subtypes or quadrants:[85]
- High neurological thresholds
- Low registration: high threshold with passive response. Individuals who do not pick up on sensations and therefore partake in passive behavior.[45]
- Sensation seeking: high threshold and active response. Those who actively seek out a rich sensory filled environment.[45]
- Low neurological threshold
- Sensitivity to stimuli: low threshold with passive response. Individuals who become distracted and uncomfortable when exposed to sensation but do not actively limit or avoid exposure to the sensation.[45]
- Sensation avoiding: low threshold and active response. Individuals actively limit their exposure to sensations and are therefore high self regulators.[45]
Sensory processing model
In Miller's nosology "sensory integration dysfunction" was renamed into "Sensory processing disorder" to facilitate coordinated research work with other fields such as neurology since "the use of the term sensory integration often applies to a neurophysiologic cellular process rather than a behavioral response to sensory input as connoted by Ayres."[5] The current nosology of sensory processing disorders was developed by Miller, based on neurological underlying principles.
Other models
A wide variety of approaches have incorporated sensation in order to influence learning and behavior.[83]
- The Alert Program for Self-Regulation is a complementary approach that encourages cognitive awareness of alertness often with the use of sensory strategies to support learning and behavior.
- Other approaches primarily use passive sensory experiences or sensory stimulation based on specific protocols, such as the Wilbarger Approach and the Vestibular-Oculomotor Protocol.
See also
References
- ↑ Cosbey J, Johnston SS, Dunn ML (2010). "Sensory processing disorders and social participation". Am J Occup Ther. 64 (3): 462–73. doi:10.5014/ajot.2010.09076. PMID 20608277.
- ↑ "Sensory Processing Disorder Explained". SPD Foundation.
- ↑ Ayres, A. Jean (1972). Sensory integration and learning disorders. Los Angeles: Western Psychological Services. ISBN 0-87424-303-3. OCLC 590960.
- ↑ Ayres AJ (1972). "Types of sensory integrative dysfunction among disabled learners". Am J Occup Ther. 26 (1): 13–8. PMID 5008164.
- 1 2 3 4 5 Miller LJ, Anzalone ME, Lane SJ, Cermak SA, Osten ET (2007). "Concept evolution in sensory integration: a proposed nosology for diagnosis" (PDF). The American Journal of Occupational Therapy. 61 (2): 135–40. doi:10.5014/ajot.61.2.135. PMID 17436834.
- ↑ Miller LJ, Nielsen DM, Schoen SA, Brett-Green BA (2009). "Perspectives on sensory processing disorder: a call for translational research". Front Integr Neurosci. 3: 22. doi:10.3389/neuro.07.022.2009. PMC 2759332
 . PMID 19826493.
. PMID 19826493. - ↑ Zimmer M, Desch L (June 2012). "Sensory integration therapies for children with developmental and behavioral disorders". Pediatrics. 129 (6): 1186–9. doi:10.1542/peds.2012-0876. PMID 22641765.
- ↑ Schaaf RC, Benevides T, Blanche EI, et al. (2010). "Parasympathetic functions in children with sensory processing disorder" (PDF). Front Integr Neurosci. 4: 4. doi:10.3389/fnint.2010.00004. PMC 2839854
 . PMID 20300470.
. PMID 20300470. - ↑ Miller, L. J.; Reisman, J. E.; McIntosh, D. N; Simon, J. S. S. Roley, E. I. Blanche, & R. C. Schaff, eds. An ecological model of sensory modulation: Performance of children with fragile X syndrome, autistic disorder, attention-deficit/hyperactivity disorder, and sensory modulation dysfunction (PDF). Understanding the nature of sensory integration with diverse populations. Tucson, AZ:: Therapy Skill Builders. pp. 75–88. ISBN 9780761615156. OCLC 46678625. Retrieved 2013-07-26.
- ↑ James K, Miller LJ, Schaaf R, Nielsen DM, Schoen SA (2011). "Phenotypes within sensory modulation dysfunction" (PDF). Compr Psychiatry. 52 (6): 715–24. doi:10.1016/j.comppsych.2010.11.010. PMID 21310399.
- ↑ Bair WN, Kiemel T, Jeka JJ, Clark JE (2012). "Development of multisensory reweighting is impaired for quiet stance control in children with developmental coordination disorder (DCD)". PLOS ONE. 7 (7): e40932. doi:10.1371/journal.pone.0040932. PMC 3399799
 . PMID 22815872.
. PMID 22815872. - ↑ Stein BE, Stanford TR, Rowland BA (December 2009). "The neural basis of multisensory integration in the midbrain: its organization and maturation". Hear. Res. 258 (1-2): 4–15. doi:10.1016/j.heares.2009.03.012. PMC 2787841
 . PMID 19345256.
. PMID 19345256. - ↑ Davies PL, Gavin WJ (2007). "Validating the diagnosis of sensory processing disorders using EEG technology". Am J Occup Ther. 61 (2): 176–89. doi:10.5014/ajot.61.2.176. PMID 17436840.
- ↑ Goldsmith, H. H.; Van Hulle, C. A.; Arneson, C. L.; Schreiber, J. E.; Gernsbacher, M. A. (2006-06-01). "A population-based twin study of parentally reported tactile and auditory defensiveness in young children". Journal of Abnormal Child Psychology. 34 (3): 393–407. doi:10.1007/s10802-006-9024-0. ISSN 0091-0627. PMC 4301432
 . PMID 16649001.
. PMID 16649001. - ↑ Davies PL, Chang WP, Gavin WJ (May 2009). "Maturation of sensory gating performance in children with and without sensory processing disorders". Int J Psychophysiol. 72 (2): 187–97. doi:10.1016/j.ijpsycho.2008.12.007. PMC 2695879
 . PMID 19146890.
. PMID 19146890. - ↑ Kisley MA, Noecker TL, Guinther PM (July 2004). "Comparison of sensory gating to mismatch negativity and self-reported perceptual phenomena in healthy adults" (PDF). Psychophysiology. 41 (4): 604–12. doi:10.1111/j.1469-8986.2004.00191.x. PMID 15189483.
- 1 2 Schneider ML, Moore CF, Gajewski LL, et al. (2008). "Sensory processing disorder in a primate model: evidence from a longitudinal study of prenatal alcohol and prenatal stress effects" (PDF). Child Dev. 79 (1): 100–13. doi:10.1111/j.1467-8624.2007.01113.x. PMID 18269511.
- ↑ Brett-Green BA, Miller LJ, Schoen SA, Nielsen DM (June 2010). "An exploratory event-related potential study of multisensory integration in sensory over-responsive children" (PDF). Brain Res. 1321: 393–407. doi:10.1016/j.brainres.2010.01.043.
- ↑ Owen, Julia P.; Marco, Elysa J.; Desai, Shivani; Fourie, Emily; Harris, Julia; Hill, Susanna S.; Arnett, Anne B.; Mukherjee, Pratik (2013). "Abnormal white matter microstructure in children with sensory processing disorders". NeuroImage: Clinical. 2: 844–853. doi:10.1016/j.nicl.2013.06.009. ISSN 2213-1582.
- ↑ Chang, Yi-Shin; Owen, Julia P.; Desai, Shivani; Hill, Susanna S.; Arnett, Anne B.; Harris, Julia; Marco, Elysa J.; Mukherjee, Pratik (2014). "Autism and Sensory Processing Disorders: Shared White Matter Disruption in Sensory Pathways but Divergent Connectivity". PLOS ONE. 9: e103038. doi:10.1371/journal.pone.0103038.
- ↑ "Breakthrough Study Reveals Biological Basis for Sensory processing disorders in Kids". UC San Francisco. Retrieved 2015-10-18.
- ↑ http://priory.com/psych/ICD.htm
- ↑ Lucy Jane Miller. "Final Decision for DSM-V". Sensory Processing Disorder Foundation. Retrieved 3 October 2013.
- ↑ Kinnealey, Moya; Miller, Lucy J (1993). Helen L Hopkins; Helen D Smith; Helen S Willard; Clare S Spackman, eds. Sensory integration and learning disabilities (PDF). Willard and Spackman's occupational therapy (8 ed.). Philadelphia: Lippincott, cop. pp. 474–489. ISBN 9780397548774. OCLC 438843342. Retrieved 2013-07-23.
- ↑ "Course information and booking". Sensory Integration Network. Retrieved 23 July 2013.
- 1 2 Eeles AL, Spittle AJ, Anderson PJ, et al. (April 2013). "Assessments of sensory processing in infants: a systematic review". Dev Med Child Neurol. 55 (4): 314–26. doi:10.1111/j.1469-8749.2012.04434.x. PMID 23157488.
- ↑ Ermer J, Dunn W (April 1998). "The sensory profile: a discriminant analysis of children with and without disabilities". Am J Occup Ther. 52 (4): 283–90. doi:10.5014/ajot.52.4.283. PMID 9544354.
- ↑ Miller-Kuhaneck H, Henry DA, Glennon TJ, Mu K (2007). "Development of the Sensory Processing Measure-School: initial studies of reliability and validity" (PDF). Am J Occup Ther. 61 (2): 170–5. doi:10.5014/ajot.61.2.170. PMID 17436839.
- ↑ Glennon, Tara J.; Miller Kuhaneck, Heather; Herzberg, David (2011). "The Sensory Processing Measure–Preschool (SPM-P)—Part One: Description of the Tool and Its Use in the Preschool Environment". Journal of Occupational Therapy, Schools, & Early Intervention. 4 (1): 42–52. doi:10.1080/19411243.2011.573245. ISSN 1941-1243.
- ↑ Wilson B1, Pollock N, Kaplan BJ, Law M, Faris P (September 1992). "Reliability and construct validity of the Clinical Observations of Motor and Postural Skills.". Am J Occup Ther. 46 (9): 775–83. doi:10.5014/ajot.46.9.775. PMID 1514563.
- ↑ Brown T, Hockey SC (January 2013). "The Validity and Reliability of Developmental Test of Visual Perception-2nd Edition (DTVP-2)". Phys Occup Ther Pediatr. 33 (4): 426–39. doi:10.3109/01942638.2012.757573. PMID 23356245.
- ↑ Deitz JC, Kartin D, Kopp K (2007). "Review of the Bruininks–Oseretsky Test of Motor Proficiency, Second Edition (BOT-2)". Phys Occup Ther Pediatr. 27 (4): 87–102. doi:10.1080/j006v27n04_06. PMID 18032151.
- ↑ Gioia GA, Isquith PK, Guy SC, Kenworthy L (September 2000). "Behavior rating inventory of executive function". Child Neuropsychol. 6 (3): 235–8. doi:10.1076/chin.6.3.235.3152. PMID 11419452.
- ↑ Gioia GA, Isquith PK, Retzlaff PD, Espy KA (December 2002). "Confirmatory factor analysis of the Behavior Rating Inventory of Executive Function (BRIEF) in a clinical sample". Child Neuropsychol. 8 (4): 249–57. doi:10.1076/chin.8.4.249.13513. PMID 12759822.
- ↑ Miller, Dr. Lucy Jane; Collins, Britt (2013). "The "So What?" of Sensory Integration Therapy: Joie de Vivre" (pdf). Sensory Solutions. Sensory Processing Disorder Foundation. Retrieved 11 January 2016.
- ↑ Baranek GT (2002). "Efficacy of sensory and motor interventions for children with autism". J Autism Dev Disord. 32 (5): 397–422. doi:10.1023/A:1020541906063. PMID 12463517.
- ↑ Schaaf RC, Miller LJ (2005). "Occupational therapy using a sensory integrative approach for children with developmental disabilities". Ment Retard Dev Disabil Res Rev. 11 (2): 143–8. doi:10.1002/mrdd.20067. PMID 15977314.
- ↑ Hodgetts S, Hodgetts W (2007). "Somatosensory stimulation interventions for children with autism: literature review and clinical considerations". Can J Occup Ther. 74 (5): 393–400. doi:10.2182/cjot.07.013. PMID 18183774.
- ↑ Nancy Peske; Lindsey Biel (2005). Raising a sensory smart child: the definitive handbook for helping your child with sensory integration issues. New York: Penguin Books. ISBN 0-14-303488-X. OCLC 56420392.
- ↑ "Sensory Checklist" (PDF). Raising a Sensory Smart Child. Retrieved 16 July 2013.
- ↑ Urwin R, Ballinger C (February 2005). "The Effectiveness of Sensory Integration Therapy to Improve Functional Behaviour in Adults with Learning Disabilities: Five Single-Case Experimental Designs". Brit J. Occupational Therapy. 68 (2): 56–66.
- ↑ Brown, Stephen; Shankar, Rohit; Smith, Kathryn (2009). "Borderline personality disorder and sensory processing impairment". Progress in Neurology and Psychiatry. 13 (4): 10–16. doi:10.1002/pnp.127. ISSN 1367-7543.
- ↑ Brown S, Shankar R, Smith K, et al. "Sensory processing disorder in mental health". Occupational Therapy News. 2006: 28–29.
- 1 2 Kinnealey, Moya; Patten Koenig, Kristie; Smith, Sinclair (2011). "Relationships Between Sensory Modulation and Social Supports and Health-Related Quality of Life". American Journal of Occupational Therapy. 65 (3): 320–327. doi:10.5014/ajot.2011.001370. PMID 21675338.
- 1 2 3 4 5 Engel-Yeger, Batya; Shochat, Tamar (June 2012). "The relationship between sensory processing patterns and sleep quality in healthy adults". Canadian Journal of Occupational Therapy. 79 (3): 134–141. doi:10.2182/cjot.2012.79.3.2.
- ↑ Carter, A. S.; A. Ben-Sasson; M. J. Briggs-Gowan (2009). "Sensory Over-Responsivity in Elementary School: Prevalence and Social-Emotional Correlates" (PDF). J Abnorm Child Psychol. 37 (5): 705–716. doi:10.1007/s10802-008-9295-8. PMID 19153827.
- ↑ Ahn, RR.; Miller, LJ.; Milberger, S.; McIntosh, DN. (2004). "Prevalence of parents' perceptions of sensory processing disorders among kindergarten children." (PDF). Am J Occup Ther. 58 (3): 287–93. doi:10.5014/ajot.58.3.287. PMID 15202626.
- 1 2 3 Ghanizadeh A (June 2011). "Sensory processing problems in children with ADHD, a systematic review". Psychiatry Investig. 8 (2): 89–94. doi:10.4306/pi.2011.8.2.89. PMC 3149116
 . PMID 21852983.
. PMID 21852983. - ↑ Lane AE, Young RL, Baker AE, Angley MT (January 2010). "Sensory processing subtypes in autism: association with adaptive behavior". J Autism Dev Disord. 40 (1): 112–22. doi:10.1007/s10803-009-0840-2. PMID 19644746.
- ↑ Tomchek SD, Dunn W (2007). "Sensory processing in children with and without autism: a comparative study using the short sensory profile". Am J Occup Ther. 61 (2): 190–200. doi:10.5014/ajot.61.2.190. PMID 17436841.
- ↑ Kern JK, Trivedi MH, Grannemann BD, et al. (March 2007). "Sensory correlations in autism". Autism. 11 (2): 123–34. doi:10.1177/1362361307075702. PMID 17353213.
- ↑ Russo N, Foxe JJ, Brandwein AB, Altschuler T, Gomes H, Molholm S (October 2010). "Multisensory processing in children with autism: high-density electrical mapping of auditory-somatosensory integration". Autism Res. 3 (5): 253–67. doi:10.1002/aur.152. PMID 20730775.
- ↑ Green SA, Ben-Sasson A (December 2010). "Anxiety disorders and sensory over-responsivity in children with autism spectrum disorders: is there a causal relationship?". J Autism Dev Disord. 40 (12): 1495–504. doi:10.1007/s10803-010-1007-x. PMC 2980623
 . PMID 20383658.
. PMID 20383658. - ↑ Baron-Cohen S, Ashwin E, Ashwin C, Tavassoli T, Chakrabarti B (May 2009). "Talent in autism: hyper-systemizing, hyper-attention to detail and sensory hypersensitivity". Philosophical Transactions of the Royal Society B. 364 (1522): 1377–83. doi:10.1098/rstb.2008.0337. PMC 2677592
 . PMID 19528020.
. PMID 19528020. - ↑ Marco EJ, Hinkley LB, Hill SS, Nagarajan SS (May 2011). "Sensory processing in autism: a review of neurophysiologic findings". Pediatr. Res. 69 (5 Pt 2): 48R–54R. doi:10.1203/PDR.0b013e3182130c54. PMC 3086654
 . PMID 21289533.
. PMID 21289533. - ↑ Cerliani L, Mennes M, Thomas R (2015). "Increased Functional Connectivity Between Subcortical and Cortical Resting-State Networks in Autism Spectrum Disorder". JAMA Psychiatry. 72: 767. doi:10.1001/jamapsychiatry.2015.0101.
- ↑ Ben-Sasson A, Hen L, Fluss R, Cermak SA, Engel-Yeger B, Gal E (2008). "A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders". J Autism Dev Disord. 39 (1): 1–11. doi:10.1007/s10803-008-0593-3. PMID 18512135.
- ↑ Williams DL, Goldstein G, Minshew NJ (2006). "Neuropsychologic functioning in children with autism: further evidence for disordered complex information-processing". Child Neuropsychol. 12 (4–5): 279–98. doi:10.1080/09297040600681190. PMC 1803025
 . PMID 16911973.
. PMID 16911973. - ↑ Baranek GT, David FJ, Poe MD, Stone WL, Watson LR (June 2006). "Sensory Experiences Questionnaire: discriminating sensory features in young children with autism, developmental delays, and typical development". J Child Psychol Psychiatry. 47 (6): 591–601. doi:10.1111/j.1469-7610.2005.01546.x. PMID 16712636.
- ↑ Little LM, Freuler AC, Houser MB, et al. (2011). "Psychometric validation of the Sensory Experiences Questionnaire". Am J Occup Ther. 65 (2): 207–10. PMC 3163482
 . PMID 21476368.
. PMID 21476368. - ↑ Lane, SJ.; Reynolds, S.; Thacker, L. (Mar 2010). "Sensory Over-Responsivity and ADHD: Differentiating Using Electrodermal Responses, Cortisol, and Anxiety.". Front Integr Neuroscience. 4. doi:10.3389/fnint.2010.00008. PMC 2885866
 . PMID 20556242.
. PMID 20556242. - ↑ Cheng, M.; Boggett-Carsjens, J. (May 2005). "Consider sensory processing disorders in the explosive child: case report and review.". Can Child Adolesc Psychiatr Rev. 14 (2): 44–8. PMC 2542921
 . PMID 19030515.
. PMID 19030515. - ↑ American Friends of Tel Aviv University (2011). "Childhood hypersensitivity linked to OCD". ScienceDaily.
- ↑ Ross LA, Saint-Amour D, Leavitt VM, Molholm S, Javitt DC, Foxe JJ (December 2007). "Impaired multisensory processing in schizophrenia: deficits in the visual enhancement of speech comprehension under noisy environmental conditions". Schizophr. Res. 97 (1-3): 173–83. doi:10.1016/j.schres.2007.08.008. PMID 17928202.
- ↑ Leavitt VM, Molholm S, Ritter W, Shpaner M, Foxe JJ (September 2007). "Auditory processing in schizophrenia during the middle latency period (10–50 ms): high-density electrical mapping and source analysis reveal subcortical antecedents to early cortical deficits". J Psychiatry Neurosci. 32 (5): 339–53. PMC 1963354
 . PMID 17823650.
. PMID 17823650. - ↑ Rabinowicz EF, Silipo G, Goldman R, Javitt DC (December 2000). "Auditory sensory dysfunction in schizophrenia: imprecision or distractibility?". Arch. Gen. Psychiatry. 57 (12): 1149–55. doi:10.1001/archpsyc.57.12.1149. PMID 11115328.
- ↑ Kratz SV (June 2009). "Sensory integration intervention: historical concepts, treatment strategies and clinical experiences in three patients with succinic semialdehyde dehydrogenase (SSADH) deficiency". J. Inherit. Metab. Dis. 32 (3): 353–60. doi:10.1007/s10545-009-1149-1. PMID 19381864.
- ↑ Tian YH, Cheng H (October 2008). "[Sensory integration function in children with primary nocturnal enuresis]". Zhongguo Dang Dai Er Ke Za Zhi (in Chinese). 10 (5): 611–3. PMID 18947482.
- ↑ Slobounov S, Tutwiler R, Sebastianelli W, Slobounov E (July 2006). "Alteration of postural responses to visual field motion in mild traumatic brain injury". Neurosurgery. 59 (1): 134–9; discussion 134–9. doi:10.1227/01.NEU.0000219197.33182.3F. PMID 16823309.
- ↑ Bharadwaj SV, Daniel LL, Matzke PL (2009). "Sensory-processing disorder in children with cochlear implants". Am J Occup Ther. 63 (2): 208–13. doi:10.5014/ajot.63.2.208. PMID 19432059.
- ↑ "Infants and Toddlers Who Require Specialty Services and Supports" (pdf). Department of Community Health—Mental Health Services to Children and Families.
- ↑ "American Psychiatric Association Board of Trustees Approves DSM-5". Retrieved 15 July 2013.
- ↑ Susan L. Hyman (2013). "New DSM-5 includes changes to autism criteria". AAP News. American Academy of Pediatrics. Retrieved 3 October 2013.
- ↑ Joanne Flanagan (2009). "Sensory processing disorder" (PDF). Pediatric News. Kennedy Krieger.org.
- 1 2 "Sensory Integration Therapies for Children With Developmental and Behavioral Disorders". Pediatrics: Official Journal of the American Academy of Pediatrics.
- ↑ Eagleman, David; Cytowic, Richard E. (2009). Wednesday is indigo blue: discovering the brain of synesthesia. Cambridge, Mass: MIT Press. ISBN 0-262-01279-0. OCLC 233697438.
- ↑ The blended senses of synesthesia, Los Angeles Times, Feb 20, 2012.
- ↑ Zamm A, Schlaug G, Eagleman DM, Loui P (July 2013). "Pathways to seeing music: enhanced structural connectivity in colored-music synesthesia". NeuroImage. 74: 359–66. doi:10.1016/j.neuroimage.2013.02.024. PMID 23454047.
- ↑ Cohen Kadosh R, Terhune DB (February 2012). "Redefining synaesthesia?". Br J Psychol. 103 (1): 20–3. doi:10.1111/j.2044-8295.2010.02003.x. PMID 22229770.
- ↑ Segal MM, Rogers GF, Needleman HL, Chapman CA (2007). "Hypokalemic sensory overstimulation". J Child Neurol. 22 (12): 1408–10. doi:10.1177/0883073807307095. PMID 18174562.
- ↑ Ayres, A. Jean.; Robbins, Jeff (2005). Sensory integration and the child : understanding hidden sensory challenge 25th Anniversary Edition. Los Angeles, CA: WPS. ISBN 978-0-87424-437-3. OCLC 63189804.
- ↑ Bundy, Anita. C.; Lane, J. Shelly; Murray, Elizabeth A. (2002). Sensory integration, Theory and practice. Philadelphia, PA: FA Davis Company. ISBN 0-8036-0545-5.
- 1 2 Smith Roley, Susanne; Zoe Mailloux; Heather Miller-Kuhaneck; Tara Glennon (September 2007). "Understanding Ayres Sensory Integration" (PDF). OT PRACTICE. 17. 12. Retrieved 19 July 2013.
- ↑ Dunn, Winnie (April 1997). "The Impact of Sensory Processing Abilities on the Daily Lives of Young Children and Their Families: A Conceptual Model". Infants & Young Children: April 1997. 9 (4). Retrieved 2013-07-19.
- ↑ Dunn W (2001). "The sensations of everyday life: empirical, theoretical, and pragmatic considerations". Am J Occup Ther. 55 (6): 608–20. doi:10.5014/ajot.55.6.608. PMID 12959225.
Further reading
- "Sensory processing disorder". Frontiers in Integrative Neuroscience – Research Topics. Retrieved 24 August 2013.
External links
- Sensory processing disorder
- STAR Center – Sensory processing disorder treatment center
- Sensory Integration Global Network
- Sensory Integration Special Interest Section
- International Training in Sensory Integration
- List of Therapists Certified in Sensory Integration including the Sensory Integration and Praxis Tests