Somnolence
| Somnolence | |
|---|---|
| Classification and external resources | |
| Specialty | Sleep medicine |
| ICD-10 | R40.0 |
| ICD-9-CM | 780.09 |
| DiseasesDB | 16940 |
| MedlinePlus | 003208 |
Somnolence (alternatively "sleepiness" or "drowsiness") is a state of strong desire for sleep, or sleeping for unusually long periods (compare hypersomnia). It has distinct meanings and causes. It can refer to the usual state preceding falling asleep,[1] the condition of being in a drowsy state due to circadian rhythm disorders, or a symptom of other health problems. It can be accompanied by lethargy, weakness, and lack of mental agility.[2]
Somnolence is often viewed as a symptom rather than a disorder by itself. However, the concept of somnolence recurring at certain times for certain reasons constitutes various disorders, such as excessive daytime sleepiness, shift work sleep disorder, and others; and there are medical codes for somnolence as viewed as a disorder.
Sleepiness can be dangerous when performing tasks that require constant concentration, such as driving a vehicle. When a person is sufficiently fatigued, microsleeps may be experienced.
The word "somnolence" is derived from the Latin "somnus" meaning "sleep."
Causes
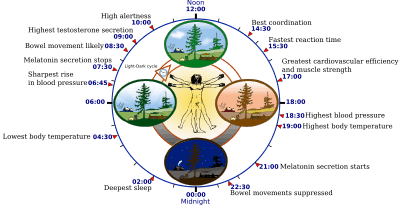
Circadian rhythm disorders
Circadian rhythm ("biological clock") disorders are a common cause of drowsiness as are a number of other conditions such as sleep apnea, insomnia, and narcolepsy.[2] The body clock disorders are classified as extrinsic (externally caused) or intrinsic. The former type is, for example, shift work sleep disorder, which affects people who work nights or rotating shifts. The intrinsic types include:[3]
- Advanced sleep phase disorder (ASPD) – A condition in which patients feel very sleepy and go to bed early in the evening and wake up very early in the morning
- Delayed sleep phase disorder (DSPD) – Faulty timing of sleep, peak period of alertness, the core body temperature rhythm, hormonal and other daily cycles such that they occur a number of hours late compared to the norm, often misdiagnosed as insomnia
- Non-24-hour sleep–wake disorder – A faulty body clock and sleep-wake cycle that usually is longer than (rarely shorter than) the normal 24-hour period causing complaints of insomnia and excessive sleepiness
- Irregular sleep–wake rhythm – Numerous naps throughout the 24-hour period, no main nighttime sleep episode and irregularity from day to day
Physical health
Sleepiness can also be a response to infection.[4] Such somnolence is one of several sickness behaviors or reactions to infection that some theorize evolved to promote recovery by conserving energy while the body fights the infection using fever and other means.[5][6] Other causes include:[7][8]
- Hypothyroidism – The body doesn't produce enough hormones that control how cells use energy
- Low blood sodium – Hyponatremia
- Hypercalcemia – Too much calcium in the blood
- Meningitis
- Head Injury
- Concussion – A mild traumatic brain injury
- Narcolepsy – Disorder of the nervous system
- Brain tumor
- Skull fractures
- Chronic pains
- Diabetes
- Fibromyalgia
- Sleeping sickness – caused by a specific parasite
- Mood disorders – Depression, Anxiety, Stress
Medications that may cause drowsiness
- analgesics – mostly prescribed or illicit opiates such as OxyContin or heroin
- anticonvulsants / antiepileptics – such as phenytoin (Dilantin), carbamazepine (Tegretol), Lyrica (pregbalin), Gabapentin
- antidepressants – for instance sedating tricyclic antidepressants,[9] and mirtazapine. Somnolence is less common with SSRIs[10] and SNRIs as well as MAOIs.
- antihistamines – for instance, diphenhydramine (Benadryl, Nytol) and doxylamine (Unisom-2)
- antipsychotics – for example, thioridazine, quetiapine (Seroquel), olanzapine (Zyprexa), risperidone, and ziprasidone (Geodon) but not haloperidol
- dopamine agonists used in the treatment of Parkinson's disease – e.g. pergolide, ropinirole and pramipexole.
- HIV medications – such as efavirenz
- hypertension medications – such as amlodipine
- tranquilizers / hypnotics – such as zopiclone (Zimovane), or the benzodiazepines such as diazepam (Valium) or nitrazepam (Mogadon) and the barbiturates, such as amobarbital (Amytal) or secobarbital (Seconal)
- other agents impacting the central nervous system in sufficient or toxic doses
Severity
A number of diagnostic tests, including the Epworth Sleepiness Scale, are available to help ascertain the seriousness and likely causes of abnormal somnolence.[11][12]
Treatment
Somnolence is a symptom, so the treatment will depend on its cause. If the cause is the behavior and life choices of the patient (like working long hours, smoking, mental state), it may help to get plenty of rest and get rid of distractions. It’s also important to investigate what’s causing the problem, such as stress or anxiety, and take steps to reduce the feeling.[7]
Associated conditions
- Alice in Wonderland syndrome
- brain edema
- cerebral hypoxia
- chronic fatigue syndrome
- circadian rhythm sleep disorders
- clinical depression, including seasonal affective disorder (SAD)
- dehydration
- diabetes – ketoacidosis as an example, but not balanced diabetes mellitus
- encephalitis – (viral, bacterial or other agents)
- epilepsy – after seizure
- fibromyalgia
- hydrocephalus
- hyperparathyroidism
- hypothermia
- hypothyroidism
- idiopathic hypersomnia
- infectious mononucleosis (glandular fever)
- intracranial hemorrhage such as due to ruptured aneurysms
- increased intracranial pressure; for example, due to brain tumors
- lyme disease (borreliosis)
- medications
- narcolepsy
- sickness behavior
- sleep apnea
- sleep deprivation
- starvation
- stroke
- traumatic brain injury
- African trypanosomiasis ("sleeping sickness")
See also
|
References
- ↑ Bereshpolova, Y.; Stoelzel, C. R.; Zhuang, J.; Amitai, Y.; Alonso, J.-M.; Swadlow, H. A. (2011). "Getting Drowsy? Alert/Nonalert Transitions and Visual Thalamocortical Network Dynamics". Journal of Neuroscience. 31 (48): 17480–7. doi:10.1523/JNEUROSCI.2262-11.2011. PMID 22131409.
- 1 2 "Drowsiness – Symptoms, Causes, Treatments". www.healthgrades.com. Retrieved 2015-10-31.
- ↑ "Circadian Sleep Disorders Network". www.circadiansleepdisorders.org. Retrieved 2015-11-02.
- ↑ Mullington, Janet; Korth, Carsten; Hermann, Dirk M.; Orth, Armin; Galanos, Chris; Holsboer, Florian; Pollmächer, Thomas (2000). "Dose-dependent effects of endotoxin on human sleep". American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 278 (4): R947–55. PMID 10749783.
- ↑ Hart, Benjamin L. (1988). "Biological basis of the behavior of sick animals". Neuroscience & Biobehavioral Reviews. 12 (2): 123–37. doi:10.1016/S0149-7634(88)80004-6. PMID 3050629.
- ↑ Kelley, Keith W.; Bluthé, Rose-Marie; Dantzer, Robert; Zhou, Jian-Hua; Shen, Wen-Hong; Johnson, Rodney W.; Broussard, Suzanne R. (2003). "Cytokine-induced sickness behavior". Brain, Behavior, and Immunity. 17 (1): 112–118. doi:10.1016/S0889-1591(02)00077-6. PMID 12615196.
- 1 2 "Drowsiness: Causes, Treatments & Prevention". www.healthline.com. Retrieved 2015-10-31.
- ↑ "Drowsiness: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Retrieved 2015-10-31.
- ↑ Zimmermann, C.; Pfeiffer, H. (2007). "Schlafstörungen bei Depression". Der Nervenarzt. 78 (1): 21–30. doi:10.1007/s00115-006-2111-1. PMID 16832696.
- ↑ Watanabe, Norio; Omori, Ichiro M; Nakagawa, Atsuo; Cipriani, Andrea; Barbui, Corrado; Churchill, Rachel; Furukawa, Toshi A (2011). "Mirtazapine versus other antidepressive agents for depression". Cochrane Database of Systematic Reviews (12): CD006528. doi:10.1002/14651858.CD006528.pub2. PMC 4158430
 . PMID 22161405.
. PMID 22161405. - ↑ Carskadon, M.A.; Dement, W.C.; Mitler, M.M.; Roth, T.; Westbrook, P.R.; Keenan, S. Guidelines for the Multiple Sleep Latency Test (MSLT): a standard measure of sleepiness. Sleep 1986; 9:519–524
- ↑ Johns, MW (March 2000). "Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the epworth sleepiness scale: failure of the MSLT as a gold standard". Journal of Sleep Research. 9 (1): 5–11. doi:10.1046/j.1365-2869.2000.00177.x. PMID 10733683.