Tropical spastic paraparesis
| Tropical spastic paraparesis | |
|---|---|
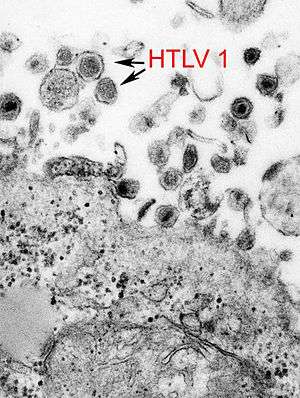 | |
| HTLV-1 which causes TSP | |
| Classification and external resources | |
| Specialty | neurology |
| ICD-10 | G04.1 |
| DiseasesDB | 29487 |
| eMedicine | med/1038 |
| Patient UK | Tropical spastic paraparesis |
| MeSH | D015493 |
Tropical spastic paraparesis (TSP), also called HTLV-I-Associated Myelopathy (HAM) or HTLV-I-Associated Myelopathy/Tropical Spastic Paraparesis (HAM/TSP)[1] is a medical condition that causes weakness, muscle spasms, and sensory disturbance by Human T-lymphotropic virus resulting in paraparesis, weakness of the legs. As the name suggests, it is most common in tropical regions, including the Caribbean.[2] Blood transfusion products are screened for HTLV-1 antibodies, as a preventive measure.[3]
Signs and symptoms
Some of the signs of Tropical spastic paraparesis are:[4]
- Leg instability
- Urinary dysfunction.
- Bowel dysfunction
- Back pain
- Erectile problems
- Psoriasis

Patients with TSP may also exhibit uveitis (inflammation of the uveal tract of the eye), arthritis (inflammation of one or more joints), pulmonary lymphocytic alveolitis (inflammation of the lung tissues), polymyositis (an inflammatory muscle disease), keratoconjunctivitis sicca (persistent dryness of the cornea and conjunctiva), and infectious dermatitis (inflammation of the skin).[5]
HTLV-1 can be transmitted via breastfeeding (mother to child), sexual contact, via blood contact (transfusion or needle sharing).[6]
Pathogenesis
In Tropical spastic paraparesis, HTLV-1 shows elevated cellular acquired immune response as well as high production of proinflammatory cytokines. IFN overexpression has been demonstrated as well. Also the number of NK cells (CD56+ and CD16+) is diminished.[7]
Diagnosis
Among the methods of diagnosing tropical spastic paraparesis are MRI (magnetic resonance imaging) and lumbar puncture (which may show lymphocytosis).[4]
Treatment

Treatment of TSP involves corticosteroids to help with inflammation. Though any success with corticosteroids is short-lived, with symptoms worsened as the dosage is reduced. A synthetic derivative, 17-alpha-ethinyltestosterone, can be used to treat Tropical spastic paraparesis, improvement in motor and bladder function was reported but not sustainable.[8]
Mogamulizumab, an anti-CCR4 IgG1 monoclonal antibody, is also being researched as a possible treatment for Tropical spastic paraparesis. The antibody reduces HTLV-1 proviral load and production of proinflammatory cytokines. Valproic acid has also succeeded in reducing the proviral load of HTLV-1 (though clinical benefits were minimal or none). A further combination of valproic acid and zidovudine has demonstrated a decrease in proviral loads (in animals).[9]
Prognosis
The prognosis for Tropical spastic paraparesis indicates some improvement in a percentage of cases due to immunosuppressive treatment. A higher percentage will eventually lose the ability to walk within a ten-year interval.[10]
History
For several decades, the term tropical spastic paraparesis was used to describe a chronic and progressive clinical syndrome that affected adults living in equatorial areas of the world. This condition was initially thought to be associated with infectious agents (such as Treponema pertenue and Treponema pallidum, which cause inflammation of the central nervous system) and with chronic nutritional deficiencies (such as avitaminosis) or exposure to potentially toxic foods (such as bitter cassava).
Tropical myeloneuropathies are classified as two separate syndromes: tropical ataxic neuropathy (TAN) and tropical spastic paraparesis (TSP). They are placed together because they are found in tropical countries, although tropical spastic paraparesis has occurred in temperate countries (e.g., Japan).[11]
References
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2610848/
- ↑ "Tropical Spastic Paraparesis Information Page: National Institute of Neurological Disorders and Stroke (NINDS)". www.ninds.nih.gov. Retrieved 2015-08-13.
- ↑ "Licensure of screening tests for antibody to human T-lymphotropic virus type I". MMWR. 37 (48): 736–40, 745–7. 1988. PMID 3143058.
- 1 2 "Tropical Spastic Paraparesis. About TSP medical condition | Patient". Patient. Retrieved 24 July 2016.
- ↑ Clarke, Charles; Howard, Robin; Rossor, Martin; Shorvon, Simon D. (2011-09-09). Neurology: A Queen Square Textbook. John Wiley & Sons. ISBN 9781444356359.
- ↑ "HTLV-1 associated myelopathy/tropical spastic paraparesis | Disease | Overview | Office of Rare Diseases Research (ORDR-NCATS)". rarediseases.info.nih.gov. Retrieved 2015-08-13.
- ↑ Yamano, Yoshihisa; Sato, Tomoo (2012). "Clinical Pathophysiology of Human T-Lymphotropic Virus-Type 1-Associated Myelopathy/Tropical Spastic Paraparesis". Frontiers in Microbiology. 3: 389. doi:10.3389/fmicb.2012.00389. PMC 3494083
 . PMID 23162542.
. PMID 23162542. - ↑ Ali, A (2006). "Tropical spastic paraparesis and polymyositis: a still unfolding story". West Indian Medical Journal. 55 (6): 459–63. doi:10.1590/S0043-31442006000600023. PMID 17691249.
- ↑ Human T-Cell Lymphotropic Viruses~treatment at eMedicine
- ↑ Prayson, Richard A. (2011-11-15). Neuropathology. Elsevier Health Sciences. ISBN 1437709494.
- ↑ Tropical Myeloneuropathies at eMedicine
Further reading
- Machigashira, N.; Yoshida, Y.; Wang, S.-y.; Osame, M. (2001). "HTLV-1-associated myelopathy/tropical spastic paraparesis with pseudohypoparathyroidism". Neurology. 56 (1): 104–6. doi:10.1212/WNL.56.1.104. PMID 11148245.
- Nagamine, Yuito; Hayashi, Takeshi; Kato, Yuji; Horiuchi, Yohsuke; Tanahashi, Norio (2015). "Human T Lymphotropic Virus Type-1-associated Myelopathy Manifesting Shortly after Living-donor Renal Transplantation". Internal Medicine. 54 (1): 75–8. doi:10.2169/internalmedicine.54.2950. PMID 25742898.