Constrictive pericarditis
| Constrictive pericarditis | |
|---|---|
 | |
| Constrictive pericarditis is defined by a fibrotic (thickened) pericardium. | |
| Classification and external resources | |
| Specialty | cardiology |
| ICD-10 | I31.1 |
| ICD-9-CM | 423.2 |
| MedlinePlus | 001103 |
| eMedicine | article/157096 |
| MeSH | D010494 |
Constrictive pericarditis is a medical condition characterized by a thickened, fibrotic pericardium, limiting the heart's ability to function normally.[1] In many cases, the condition continues to be difficult to diagnose and therefore benefits from a good understanding of the underlying cause.[2]
Symptoms
Symptoms of constrictive pericarditis are consistent with the following: fatigue, swollen abdomen, difficulty breathing (dyspnea), swelling of legs and general weakness. Related conditions are bacterial pericarditis, pericarditis and pericarditis after a heart attack.[1]
Causes
The cause of constrictive pericarditis in the developing world are idiopathic in origin, though likely infectious in nature. In regions where tuberculosis is common, it is the cause in a large portion of cases.[3]
Causes of constrictive pericarditis include:
- Tuberculosis[4]
- Incomplete drainage of purulent pericarditis[4]
- Fungal and parasitic infections[4]
- Chronic pericarditis[4]
- Postviral pericarditis[4]
- Postsurgical[4]
- Following MI, post-myocardial infarction[4]
- In association with pulmonary asbestos[5]
Pathophysiology
The pathophysiological characteristics of constrictive pericarditis are due to a thickened, fibrotic pericardium that forms a non-compliant shell around the heart. This shell prevents the heart from expanding when blood enters it. This results in significant respiratory variation in blood flow in the chambers of the heart.[6]
During inspiration, pressure in the thoracic cavity decreases but is not relayed to the left atrium, subsequently a reduction in flow to the left atrium and ventricle happens. During diastole, less blood flow in left ventricle allows for more room for filling in right ventricle and therefore a septal shift occurs.[7]
During expiration, the amount of blood entering the right ventricle will decrease, allowing the interventricular septum to bulge towards the right ventricle, and increased filling of the left ventricle and subsequent increased pressure generated by the left ventricle during systole.This is known as ventricular interdependence, since the amount of blood flow into one ventricle is dependent on the amount of blood flow into the other ventricle.
Diagnosis
The diagnosis of constrictive pericarditis is often difficult to make. In particular, restrictive cardiomyopathy has many similar clinical features to constrictive pericarditis, and differentiating them in a particular individual is often a diagnostic dilemma.[8]
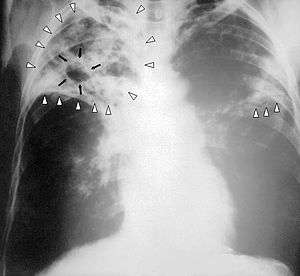
- Chest X-Ray - pericardial calcification (common but not specific), pleural effusions are common findings.[9]
- Echocardiography - the principal echographic finding is changes in cardiac chamber volume.[9]
- CT and MRI - useful in select cases.[9]
- BNP blood test - tests for the existence of the cardiac hormone brain natriuretic peptide, which is only present in RCMP but not in CP[10]
- Conventional cardiac catheterization[11]
- Physical examination -can reveal clinical features including Kussmaul's sign and a pericardial knock.[11]
Treatment
The definitive treatment for constrictive pericarditis is pericardial stripping, which is a surgical procedure where the entire pericardium is peeled away from the heart. This procedure has significant risk involved,[12] with mortality rates of 6% or higher in major referral centers.[13]
A poor outcome is almost always the result after a pericardiectomy is performed for constrictive pericarditis whose origin was radiation-induced,further some patients may develop heart failure post-operatively.[14]
References
- 1 2 "Contrictive pericarditis". Medline Plus. NIH. Retrieved 21 September 2015.
- ↑ Schwefer, Markus; Aschenbach, Rene; Heidemann, Jan; Mey, Celia; Lapp, Harald (September 2009). "Constrictive pericarditis, still a diagnostic challenge: comprehensive review of clinical management". European Journal of Cardio-Thoracic Surgery. 36 (3): 502–510. doi:10.1016/j.ejcts.2009.03.004. Retrieved 21 September 2015.
- ↑ Dunn, editor, Brian P. Griffin ; associate editors, Thomas D. Callahan, Venu Menon ; guest editors, Willis M. Wu, Clay A. Cauthen, Justin M. (2013). Manual of cardiovascular medicine (4th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 653. ISBN 978-1-4511-3160-4. Retrieved 21 September 2015.
- 1 2 3 4 5 6 7 "Constritive pericarditis". eMedicine. MedScape. Retrieved 21 September 2015.
- ↑ Lloyd, editors-in-chief, Joseph G. Murphy, Margaret A. (2013). Mayo Clinic cardiology : concise textbook (4th ed.). Oxford: Mayo Clinic Scientific Press/Oxford University Press. p. 718. ISBN 978-0-199915712. Retrieved 21 September 2015.
- ↑ Crouch, [edited by] Michael A. (2010). Cardiovascular pharmacotherapy : a point-of-care guide. Bethesda, Md.: American Society of Health-System Pharmacists. p. 376. ISBN 978-1-58528-215-9. Retrieved 21 September 2015.
- ↑ Camm, Demosthenes G. Katritsis, Bernard J. Gersh, A. John (2013). Clinical cardiology : current practice guidelines (1st ed.). Oxford: Oxford University Press. p. 388. ISBN 978-0-19-968528-8. Retrieved 21 September 2015.
- ↑ "Restrictive pericarditis". eMedicine. MedScape. Retrieved 21 September 2015.
- 1 2 3 "Imaging in Constrictive pericarditis". eMedicine. MedScape. Retrieved 21 September 2015.
- ↑ Semrad, Michal (2014). Cardiovascular Surgery. Charles University. p. 114. ISBN 978-80-246-2465-5. Retrieved 21 September 2015.
- 1 2 Khandaker, Masud H.; Espinosa, Raul E.; Nishimura, Rick A.; Sinak, Lawrence J.; Hayes, Sharonne N.; Melduni, Rowlens M.; Oh, Jae K. (June 2010). "Pericardial Disease: Diagnosis and Management". Mayo Clinic Proceedings. 85 (6): 572–593. doi:10.4065/mcp.2010.0046. PMC 2878263
 . PMID 20511488.
. PMID 20511488. - ↑ Cinar B, Enc Y, Goksel O, Cimen S, Ketenci B, Teskin O, Kutlu H, Eren E (2006). "Chronic constrictive tuberculous pericarditis: risk factors and outcome of pericardiectomy". Int J Tuberc Lung Dis. 10 (6): 701–6. PMID 16776460.
- ↑ Chowdhury UK, Subramaniam GK, Kumar AS, Airan B, Singh R, Talwar S, Seth S, Mishra PK, Pradeep KK, Sathia S, Venugopal P (2006). "Pericardiectomy for constrictive pericarditis: a clinical, echocardiographic, and hemodynamic evaluation of two surgical techniques". Ann Thorac Surg. 81 (2): 522–9. doi:10.1016/j.athoracsur.2005.08.009. PMID 16427843.
- ↑ Greenberg, editors, Jeffrey D. Hosenpud, Barry H. (2007). Congestive heart failure (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 410. ISBN 0-7817-6285-5. Retrieved 21 September 2015.
Further reading
- Smiseth, Otto A.; (eds.), Michał Tendera (2008). Diastolic heart failure. London: Springer. ISBN 978-1-84628-890-6. Retrieved 21 September 2015.
- Hoit, B. D. (25 June 2002). "Management of Effusive and Constrictive Pericardial Heart Disease". Circulation. 105 (25): 2939–2942. doi:10.1161/01.CIR.0000019421.07529.C5. Retrieved 21 September 2015.