Salivary gland pathology
| Salivary gland disease | |
|---|---|
| Classification and external resources | |
| MeSH | D012466 |
Salivary gland diseases (sometimes abbreviated to SGD),[1] are multiple and varied in etiology.
There are 3 paired major salivary glands in humans (the parotid gland, the submandibular gland, and the sublingual gland), as well as about 800-1000 minor salivary glands in the oral mucosa of the mouth. The parotid gland is located in front of the ear, and it secretes its mostly serous saliva via the parotid duct (Stenson duct) into the mouth, usually opening roughly opposite the maxillary second molar. The submandibular gland is located medial to the angle of the mandible, and it drains its mixture of serous and mucous saliva via the submandibular duct (Wharton duct) into the mouth, usually opening in a punctum located in the floor of mouth. The sublingual gland is located below the tongue, in the floor of the mouth. It drains its mostly mucous saliva into the mouth via about 8-20 ducts which open along the plica sublingualis (a fold of tissue under the tongue).[2]
The function of the salivary glands is to secrete saliva, which has a lubricating function, which protects the oral mucosa of the mouth during eating and speaking.[2] Saliva also contains digestive enzymes (e.g. salivary amylase) and has antimicrobial action and acts as a buffer. Persons with reduced salivary flow or hyposalivation often suffer from dry mouth or xerostomia, which can result in severe dental caries (tooth decay) as a result of the loss of the protective effects of saliva.
Various examples of disorders affecting the salivary glands are listed below. Some are more common than others, and they are considered according to a surgical sieve, but this list is not exhaustive. Sialadenitis is inflammation of a salivary gland, usually caused by infections, although there are other less common causes of inflammation such as irradiation, allergic reactions or trauma.[3]
Congenital
Congenital disorders of the salivary glands are rare,[3] but may include:
- Aplasia
- Atresia
- Ectopic salivary gland tissue
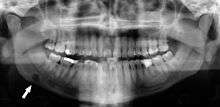
- Stafne defect - an uncommon condition which some consider to be an anatomic variant rather than a true disease. It is thought to be created by an ectopic portion of salivary gland tissue which causes the bone of the mandible to remodel around the tissue, creating an apparent cyst like radiolucent area on radiographs. Classically, this lesion is discovered as a chance finding,[4] since it causes no symptoms. It appears below the inferior alveolar nerve canal in the posterior region of the mandible.
Acquired
Vascular
- Necrotizing sialometaplasia—a lesion that usually arises from a minor salivary gland on the palate. It is thought to be due to vascular infarction of the salivary gland lobules. It is often mistaken for oral cancer, but the lesion is not neoplastic.[2]
Infective
Infections involving the salivary glands can be viral or bacterial (or rarely fungal).
- Mumps is the most common viral sialadenitis. It usually occurs in children, and there is preauricular pain (pain felt in front of the ear), swelling of the parotid, fever, chills, and headaches.[2]
- Bacterial sialadentitis is usually caused by ascending organisms from the oral cavity. Risk factors include reduced salivary flow rate.
- Human immunodeficiency virus-associated salivary gland disease (HIV-SGD).[1]
Traumatic

- Mucocele — these are common and are caused by rupture of a salivary gland duct and mucin spillage into the surrounding tissues. Usually they are caused by trauma. Classically, a mucocele is blusish and fluctuant, and most commonly occurs on the lower lip.[5]
- Ranula — the name used when a mucocele occurs in the floor of the mouth (underneath the tongue). Ranulas may grow to a larger size than mucoceles at other sites, and they are usually associated with the sublingual gland, although less commonly they may also arise from the submandibular gland or a minor salivary gland.[5] Uncommonly, a ranula may descend into the neck rather than the mouth (plunging ranula). If small, the ranula may be left alone, but if larger and causing symptoms, excision of the sublingual gland may be indicated.
- Nicotinic stomatitis — the hard palate is whitened by hyperkeratosis caused by the heat from tobacco use or hot liquid consumption. This irritation also causes inflammation of the duct openings of the minor salivary glands of the palate, and they become dilated. This manifests as red patches or spots on a white background.[6]
Autoimmune
Inflammatory
- Post-irradiation sialadenitis
- Sarcoidosis—there may be parotitis alone or uveoparotitis (inflammation of both the parotid and the uvea of the eyes), which occurs in Heerfordt's syndrome.
- Cheilitis glandularis—This is inflammation of the minor salivary glands, usually in the lower lip, eversion and swelling of the lip.[5]
- Chronic sclerosing sialadenitis is a salivary gland manifestation of IgG4-related disease.[7][8]
Neurological
Neoplastic
Idiopathic
- Sialolithiasis - although several possibly coexisting factors have been suggested to be involved in the formation of salivary stones, including altered acidity of saliva, reduced salivary flow rate, abnormal calcium metabolism and abnormalities in the sphincter mechanism of the duct opening, the exact cause in many cases is unknown.
- Sialadenosis (sialosis) is an uncommon, non-inflammatory, non-neoplastic, recurrent swelling of the salivary glands. The cause is hypothesized to be abnormalities of neurosecretory control. It may be associated with alcoholism.[3][9][10]
References
- 1 2 Jeffers, L; Webster-Cyriaque, JY (April 2011). "Viruses and salivary gland disease (SGD): lessons from HIV SGD.". Advances in Dental Research. 23 (1): 79–83. doi:10.1177/0022034510396882. PMC 3144046
 . PMID 21441486.
. PMID 21441486. - 1 2 3 4 Hupp JR, Ellis E, Tucker MR (2008). Contemporary oral and maxillofacial surgery (5th ed.). St. Louis, Mo.: Mosby Elsevier. pp. 397–419. ISBN 9780323049030.
- 1 2 3 Soames JV, Southam JC, JV (1999). Oral pathology (3rd ed.). Oxford: Oxford Univ. Press. pp. 247–265. ISBN 0192628941.
- ↑ Wray D, Stenhouse D, Lee D, Clark AJ (2003). Textbook of general and oral surgery. Edinburgh [etc.]: Churchill Livingstone. pp. 236–237. ISBN 0443070830.
- 1 2 3 Neville BW, Damm DD, Allen CA, Bouquot JE (2002). Oral & maxillofacial pathology (2nd ed.). Philadelphia: W.B. Saunders. pp. 389–430. ISBN 0721690033.
- ↑ Illustrated Dental Embryology, Histology, and Anatomy, Bath-Balogh and Fehrenbach, Elsevier, 2011, page 137
- ↑ John H. Stone; Arezou Khosroshahi; Vikram Deshpande; et al. (October 2012). "Recommendations for the nomenclature of IgG4-related disease and its individual organ system manifestations". Arthritis & Rheumatism. 64 (10): 3061–3067. doi:10.1002/art.34593. PMID 22736240.
- ↑ Aly, Fatima (2011-10-07). "Salivary glands: Inflammation: Sialadenitis". Pathology Outlines. Retrieved 2013-12-05.
- ↑ Pape, SA; MacLeod, RI; McLean, NR; Soames, JV (September 1995). "Sialadenosis of the salivary glands.". British journal of plastic surgery. 48 (6): 419–22. doi:10.1016/s0007-1226(95)90233-3. PMID 7551515.
- ↑ Mandel, L; Hamele-Bena, D (October 1997). "Alcoholic parotid sialadenosis.". Journal of the American Dental Association (1939). 128 (10): 1411–5. doi:10.14219/jada.archive.1997.0060. PMID 9332142.
External links
| Wikimedia Commons has media related to Pathology of the salivary glands. |