Steroid hormone
A steroid hormone is a steroid that acts as a hormone. Steroid hormones can be grouped into 2 classes, corticosteroids (typically made in the adrenal cortex, hence cortico-) and sex steroids (typically made in the gonads or placenta). Within those 2 classes are 5 types according to the receptors to which they bind: glucocorticoids and mineralocorticoids (corticosteroids) and androgens, estrogens, and progestogens (sex steroids). Vitamin D derivatives are a sixth closely related hormone system with homologous receptors. They have some of the characteristics of true steroids as receptor ligands.
Steroid hormones help control metabolism, inflammation, immune functions, salt and water balance, development of sexual characteristics, and the ability to withstand illness and injury. The term steroid describes both hormones produced by the body and artificially produced medications that duplicate the action for the naturally occurring steroids.[1][2][3]
Synthesis
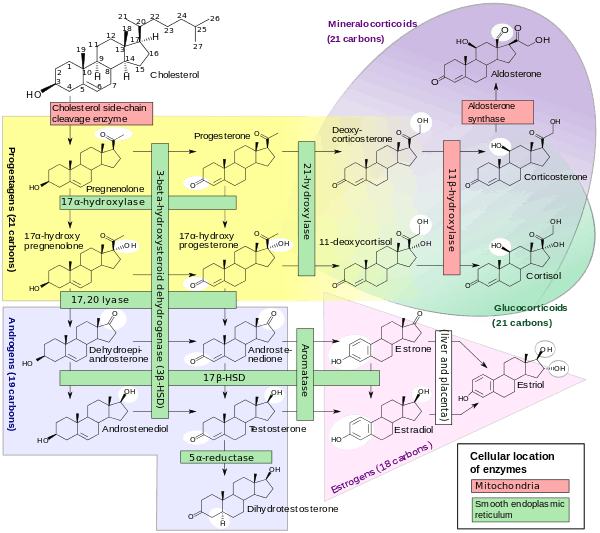
The natural steroid hormones are generally synthesized from cholesterol in the gonads and adrenal glands. These forms of hormones are lipids. They can pass through the cell membrane as they are fat-soluble,[5] and then bind to steroid hormone receptors (which may be nuclear or cytosolic depending on the steroid hormone) to bring about changes within the cell. Steroid hormones are generally carried in the blood, bound to specific carrier proteins such as sex hormone-binding globulin or corticosteroid-binding globulin. Further conversions and catabolism occurs in the liver, in other "peripheral" tissues, and in the target tissues.
Synthetic steroids and sterols
A variety of synthetic steroids and sterols have also been contrived. Most are steroids, but some non-steroidal molecules can interact with the steroid receptors because of a similarity of shape. Some synthetic steroids are weaker or stronger than the natural steroids whose receptors they activate.[6]
Some examples of synthetic steroid hormones:
- Glucocorticoids: alclometasone, prednisone, dexamethasone, triamcinolone, cortisone
- Mineralocorticoid: fludrocortisone
- Vitamin D: dihydrotachysterol
- Androgens: apoptone, oxandrolone, oxabolone, testosterone, nandrolone (also known as anabolic steroids)
- Oestrogens: diethylstilbestrol (DES) and beta estradiol
- Progestins: danazol, norethisterone, medroxyprogesterone acetate, 17-hydroxyprogesterone caproate.
Some steroid antagonists:
- Androgen: cyproterone acetate
- Progestins: mifepristone, gestrinone
Transport
Steroid hormones are transported through the blood by being bound to carrier proteins—serum proteins that bind them and increase the hormones' solubility in water. Some examples are sex hormone-binding globulin (SHBG), corticosteroid-binding globulin, and albumin.[7] One study has found that these steroid-carrier complexes may be taken into cells via endocytosis, whereon the steroids are released and interact with intracellular proteins to bring about changes in the target cell.[8] However, most studies say that hormones generally act only when they are not bound by serum proteins. This is known as the free hormone hypothesis. This hypothesis claims that in order to be active, steroid hormones must free themselves from their blood-solubilizing proteins and either bind to extracellular receptors, or passively cross the cell membrane and bind to nuclear receptors.
In order for steroid hormones to cross the lipid bilayer of cells they must overcome energetic barriers that would prevent their entering or exiting the membrane. These hormones, which are all derived from cholesterol, have hydrophilic functional groups at either end, and a hydrophobic carbon backbone. Relative to crossing a membrane, the free energy barriers exist when the functional groups are entering the hydrophobic interior of membrane, or when the hydrophobic portion of the steroids reintroduced to an aqueous environment on either side of the membrane. Many molecules have enough energy to enter and exit the membrane at physiologic conditions, and they have experimentally been shown to cross membranes near a rate of 20 μm/s, depending on the molecule.[9]
What may be more interesting, is that the hormones do in fact leave the membrane once they have entered it. This is an important consideration because cholesterol—the precursor to all steroid hormones—does not leave the membrane once it has embedded itself inside. The difference between cholesterol and these hormones is that cholesterol is in a much larger negative Gibb's free energy well once inside the membrane, as compared to these hormones.[9]
Mechanisms of Action and Effects
There are many different mechanisms through which steroid hormones affect their target cells. All of these different pathways can be classified as having either a genomic effect, or a non-genomic effect. Genomic pathways are slow and result in altering transcription levels of certain proteins in the cell; non-genomic pathways are much faster.
Genomic Pathways
The first identified mechanisms of steroid hormone action were the genomic effects.[10] In this pathway, the free hormones first pass through the cell membrane because they are fat soluble.[5] In the cytoplasm, the steroid may or may not undergo an enzyme-mediated alteration such as reduction, hydroxylation, or aromatization. Also in the cytoplasm, the steroid binds to a specific steroid hormone receptor, also known as a nuclear receptor, which is a large metalloprotein. Upon steroid binding, many kinds of steroid receptors dimerize: two receptor subunits join together to form one functional DNA-binding unit that can enter the cell nucleus. Once in the nucleus, the steroid-receptor ligand complex binds to specific DNA sequences and induces transcription of its target genes.[2][11][12][13]
Non-genomic Pathways
Because non-genomic pathways include any mechanism that is not a genomic effect, there are various non-genomic pathways. However, all of these pathways are mediated by some type of receptor found at the plasma membrane.[14] Ion channels, transporters, G-protein coupled receptors (GPCR), and membrane fluidity have all been shown to be affected by steroid hormones.[9] Of these, GPCR linked proteins are the most common.
GPCR linked proteins most likely interact with steroid hormones through an amino acid consensus sequence traditionally thought of as a cholesterol recognition and interaction site. About a third of Class A GPCRs contain this sequence. The steroid hormones themselves are different enough from one another that they do not all affect all of the GPCR linked proteins; however, the similarities between the steroid hormones and between the receptors make plausible the argument that each receptor may respond to multiple steroid hormones or that each hormone could affect multiple receptors. This is contrary to the traditional model of having a unique receptor for each unique ligand.[15]
At least four different GPCR-linked proteins are known to respond to steroid hormones. G Protein-Coupled Receptor 30 (GPR30) binds estrogen, Membrane Progestin Receptor (mPR) binds progesterone, G Protein-Coupled Receptor Family C Group 6 Member A (GPRC6A) binds androgens, and Thyroid Hormone and Trace Amine Associated Receptor 1 (TAAR1) binds Thyroid hormone (though not technically steroid hormones, thyroid hormones can be grouped here because their receptors belong to the nuclear receptor superfamily). As an example of the effects of these GPCR-linked proteins consider GPR30. GPR30 binds estrogen, and upon binding estrogen this pathway activates adenylyl cyclase and epidermal growth factor receptor. It results in vasodilation, renoprotection, mammary gland development, etc.[15]
See also
References
- ↑ Funder JW, Krozowski Z, Myles K, Sato A, Sheppard KE, Young M (1997). "Mineralocorticoid receptors, salt, and hypertension". Recent Prog Horm Res. 52: 247–260. PMID 9238855.
- 1 2 Gupta BBP, Lalchhandama K (2002). "Molecular mechanisms of glucocorticoid action" (PDF). Current Science. 83 (9): 1103–1111.
- ↑ Frye CA (2009). "Steroids, reproductive endocrine function, and affect. A review". Minerva Ginecol. 61 (6): 541–562. PMID 19942840.
- ↑ Häggström, Mikael; Richfield, David (2014). "Diagram of the pathways of human steroidogenesis". WikiJournal of Medicine. 1 (1). doi:10.15347/wjm/2014.005. ISSN 2002-4436.
- 1 2 Linda J. Heffner; Danny J. Schust (2010). The Reproductive System at a Glance. John Wiley and Sons. pp. 16–. ISBN 978-1-4051-9452-5. Retrieved 28 November 2010.
- ↑ Nahar L, Sarker SD, Turner AB (2007). "A review on synthetic and natural steroid dimers: 1997-2006". Curr Med Chem. 14 (12): 1349–1370. doi:10.2174/092986707780597880. PMID 17504217.
- ↑ Adams, John S. 2005. "Bound" to work: The free hormone hypothesis revisited. Cell 122 (5): 647-9.
- ↑ Hammes, A. 2005. Role of endocytosis in cellular uptake of sex steroids. Cell 122 (5): 751-62.
- 1 2 3 Oren, Idit. 2004. Free diffusion of steroid hormones across biomembranes: A simplex search with implicit solvent model calculations. Biophysical Journal 87 (2): 768-79.
- ↑ Rousseau, Guy. 2013. Fifty years ago: The quest for steroid hormone receptors. Molecular and Cellular Endocrinology 375 (1-2): 10-3.
- ↑ Moore FL, Evans SJ (1995). "Steroid hormones use non-genomic mechanisms to control brain functions and behaviors: a review of evidence". Brain Behav Evol. 51 (4): 41–50. PMID 10516403.
- ↑ Marcinkowska E, Wiedłocha A (2002). "Steroid signal transduction activated at the cell membrane: from plants to animals". Acta Biochim Pol. 43 (9): 735–745. PMID 12422243.
- ↑ Rousseau GG (2013). "Fifty years ago: The quest for steroid hormone receptors". Mol Cell Endocrinol. 375 (1–2): 10–13. doi:10.1016/j.mce.2013.05.005. PMID 23684885.
- ↑ G-PROTEINCOUPLEDRECEPTORS
- 1 2 Wang, Chen, Yi Liu, and Ji-Min Cao. 2014. G protein-coupled receptors: Extranuclear mediators for the non-genomic actions of steroids. International Journal of Molecular Sciences 15 (9): 15412-25.
Further reading
- Brook CG. Mechanism of puberty. Horm Res. 1999;51 Suppl 3:52–4. Review.PMID 10592444
- Holmes SJ, Shalet SM. Role of growth hormone and sex steroids in achieving and maintaining normal bone mass. Horm Res. 1996;45(1–2):86–93. Review. PMID 8742125
- Ottolenghi C, Uda M, Crisponi L, Omari S, Cao A, Forabosco A, Schlessinger D. Determination and stability of sex. Bioessays. 2007 Jan;29(1):15–25. Review. PMID 17187356
- Couse JF, Korach KS. Exploring the role of sex steroids through studies of receptor deficient mice. J Mol Med. 1998 Jun;76(7):497–511. Review. PMID 9660168
- McEwen BS. Steroid hormones: effect on brain development and function. Horm Res. 1992;37 Suppl 3:1–10. Review. PMID 1330863
- Simons SS Jr. What goes on behind closed doors: physiological versus pharmacological steroid hormone actions. Bioessays. 2008 Aug;30(8):744–56. PMID 18623071
- Han, Thang S.; Walker, Brian R.; Arlt, Wiebke; Ross, Richard J. (17 December 2013). "Treatment and health outcomes in adults with congenital adrenal hyperplasia". Nature Reviews Endocrinology. 10 (2): 115–124. doi:10.1038/nrendo.2013.239. PMID 24342885Figure 2: The adrenal steroidogenesis pathway.
External links
- An animated and narrated tutorial about nuclear receptor signaling
- Virtual Chembook
- stedwards.edu
- How Steroid Hormones Work