Sufentanil
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Sufenta |
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration | IV, IM, SubQ, epidural, intrathecal, transdermal patch (in clinical trials) |
| ATC code | N01AH03 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Biological half-life | 162 minutes |
| Duration of action | 30 to 60 min[1] |
| Identifiers | |
| |
| CAS Number |
56030-54-7 |
| PubChem (CID) | 41693 |
| IUPHAR/BPS | 3534 |
| DrugBank |
DB00708 |
| ChemSpider |
38043 |
| UNII |
AFE2YW0IIZ |
| KEGG |
D05938 |
| ChEBI |
CHEBI:9316 |
| ChEMBL |
CHEMBL658 |
| ECHA InfoCard | 100.168.858 |
| Chemical and physical data | |
| Formula | C22H30N2O2S |
| Molar mass | 386.552 g/mol |
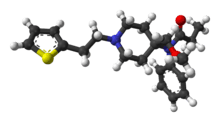
| 3D model (Jmol) | Interactive image |
| Melting point | 97 °C (207 °F) |
| |
| |
| (verify) | |
Sufentanil (R30730, brand name Sufenta) is a synthetic opioid analgesic drug approximately five to 10 times more potent than its parent drug, fentanyl, and 500 times as potent as morphine. Structurally, sufentanil differs from fentanyl through the addition of a methoxy group on the piperidine ring (which is believed to reduce duration of action[2]), and the replacement of the phenyl ring by thiophene. Sufentanil first was synthesized at Janssen Pharmaceutica in 1974.[3]
Sufentanil is marketed for use by specialist centers under different trade names, such as Sufenta and Sufentil. Sufentanil with and without lidocaine or mepivacaine is available as a transdermal patch similar to Duragesic in Europe under trade names such as Chronogesic.
Uses
The main use of this medication is in operating suites and critical care where pain relief is required for a short period of time. It also offers properties of sedation and this makes it a good analgesic component of anesthetic regimen during an operation.[4] It is usually administered under the doctor's order through an intravenous route. In some countries, sufentanil is only indicated for epidural use. Despite this, it is often used off-label both intravenously and intranasally. A transdermal sufentanil patch called Transdur-sufentanil is about to enter Stage III clinical trials by Durect Corp for the relief of chronic pain, and has the advantage over fentanyl patches such as Duragesic of only needing to be applied once per week. Sufentanil is also used off-label in intrathecal pumps.
Because of its extremely high potency, it is often used in surgery and post-operative pain management for patients that are heavily opioid dependent/opioid tolerant because of long term opiate use for chronic pain or illicit opiate use. Currently sufentanil is the strongest opioid painkiller available for use in humans. Although stronger narcotic pain medications do exist, all medications stronger than sufentanil are approved for veterinary use only. It is also used in surgery and post operative pain control in patients that are taking high dose buprenorphine for chronic pain because it is the only opioid that has a potency and binding affinity strong enough to displace buprenorphine from the opioid receptors in the central nervous system and provide analgesia.[5][6]
Side effects
It is essential for the administering medical professional to be trained in airway management with readily available airway equipment because the drug causes significant respiratory depression and may cause respiratory arrest if given too rapidly or in too high a dose. Other opioid side effects such as heart rhythm irregularity, blood pressure changes and nausea/vomiting can also be present in patients given this drug and should be dealt with accordingly.
Sufentanil has been associated with extremely rare instances of life-threatening anaphylaxis.
Overdose management
Because sufentanil is very potent, practitioners must be prepared to reverse the effects of the drug should the patient exhibit symptoms of overdose such as respiratory depression or respiratory arrest. As for all other opioid-based medications, naloxone (trade name Narcan) is the definitive antidote for overdose. Depending on the amount administered, it can reverse the respiratory depression and, if enough is administered, completely reverse the effects of sufentanil. In these situations, doctors will normally only administer enough naloxone to reverse the respiratory depression to the point where the patient begins breathing on their own again. Completely reversing the effects of the sufentanil would result in the patient being suddenly forced into opiate withdrawal and all of the negative side effects that come with it.[7][8]
See also
References
- ↑ Shaw, Leslie M. (2001). The clinical toxicology laboratory : contemporary practice of poisoning evaluation. Washington, DC: AACC Press. p. 89. ISBN 9781890883539.
- ↑ Vucković S, Prostran M, Ivanović M, Dosen-Mićović Lj, Todorović Z, Nesić Z, Stojanović R, Divac N, Miković Z (2009). "Fentanyl analogs: structure-activity-relationship study.". Curr Med Chem. 16 (9): 2468–2474. PMID 19601792.
- ↑ Niemegeers CJ, Schellekens KH, Van Bever WF, Janssen PA (1976). "Sufentanil, a very potent and extremely safe intravenous morphine-like compound in mice, rats and dogs". Arzneimittel-Forschung. 26 (8): 1551–6. PMID 12772.
- ↑ Savoia G, Loreto M, Gravino E (September 2001). "Sufentanil: an overview of its use for acute pain management". Minerva Anestesiologica. 67 (9 Suppl 1): 206–216. PMID 11778119.
- ↑ "Fentanyl Citrate - Drug Summary - PDR.net". pdr.net. Retrieved 23 October 2015.
- ↑ Buprenorphine
- ↑ "Sufenta (Sufentanil Citrate Injection) Drug Information: Overdosage and Contraindications - Prescribing Information at RxList". RxList. Retrieved 23 October 2015.
- ↑ "The First and Only Naloxone Auto-Injector EVZIO® (naloxone HCl injection)". evzio.com. Retrieved 23 October 2015.