GABAA receptor positive allosteric modulator

In pharmacology, GABAA receptor positive allosteric modulators are positive allosteric modulator (PAM) molecules that increase the activity of the GABAA receptor protein in the vertebrate central nervous system. Unlike GABAA receptor agonists, GABAA PAMs do not bind at the same active site as the γ-Aminobutyric acid (GABA) neurotransmitter molecule: PAMs affect the receptor by binding at a different site on the protein. This is called allosteric modulation.
GABA is a major inhibitory neurotransmitter in the central nervous system. Upon binding, it triggers the GABAA receptor to open its chloride channel to allow chlorine ions into the neuron, making the cell hyperpolarized and less likely to fire. GABAA PAMs bind to a different site and increase the effect of GABA by making the channel open more frequently or for longer when GABA binds. However, they do not have an effect if GABA or another agonist is not present.
In psychopharmacology, GABAA receptor PAMs used as drugs have mainly sedative and anxiolytic effects. Examples of GABAA PAMs include alcohol (ethanol), benzodiazepines such as diazepam (Valium) and alprazolam (Xanax), Z-drugs such as zolpidem (Ambien), and the barbiturate drugs.
History
The GABAA receptors have been historically a target of several drug treatment research. The earliest compounds were ions, like for example bromide.
In 1903, the first psychoactive derivative of barbituric acid was synthesized and marketed for headaches. Within 30 years, many other barbiturates were developed and found use as sedatives, sleep aids and general anesthetics. Although barbiturates are rarely used today, they continue to serve as a short-acting anesthetics and anti-epileptic drugs.
Benzodiazepines were discovered in 1950 and largely replaced the barbiturates because of larger therapeutical index.[1] At first benzodiazepines were considered to be very safe and very efficient minor tranquilizers but later they were criticized for their dependence producing effects. Currently there are several efficient benzodiazepines available and so one can be selected in relation to its dosage form, length of action, metabolic interaction and safety as needed. Benzodiazepines function by binding to the benzodiazepine site on most, but not all, GABAA receptors. GABAA modulation by benzodiazepine site agonists is self-limiting and the conductance of the channel is not higher with the presence of benzodiazepine and GABA than the conductane with the presence of only high concentration of GABA. Additionally, in the absence of GABA the presence of benzodiazepines alone does not open the chloride channel.[2]
Certain metabolites of progesterone and deoxycorticosterone are established as potent and selective positive allosteric modulators of the γ-aminobutyric acid type A (GABAA) receptor.[3] Hans Selye demonstrated in the 1940 that certain pregnane steroids could cause both anesthesia and sedation[4] but it was not until 40 years later that molecular mechanism emerged to explain the depressant effect of these steroids. In a rat brain slice preparation, the synthetic steroidal anesthetic alphaxalone (5α-pregnan-3α-ol-11,20 dione) enhanced both stimulus-evoked inhibition and the effects of exogenously applied muscimol which is a GABAA selective agonist.[5]
Receptor

The GABAA receptors are made up of subunits which form a receptor complex. The receptor subunits in humans are 19 and are classified into α (1–6), β (1–3), γ (1–3), δ, ε, π, θ, and ρ (1−3). The function of the receptor is different according to how the pentameric complex is put together. The most common complex which includes around 40% of the GABAA receptors is the α1β2γ2 combination. The expression of the subunits can be very different depending on brain region.[6] The combination of the subunits influences how the receptor acts. For example if the α1 and β2 subunits are expressed together they have high sensitivity to GABA but low channel conductance. But if the γ2 is expressed with α1 and β2 the sensitivity is low and channel conductance is high.[7] γ2 subunit has to be present for high affinity binding of benzodiazepine. The knowledge on where different complexes are located in the brain is still minimal. That makes it hard to develop drugs for certain regions.[6] For example the binding site of neurosteroids in the GABAA receptor is not known[8] and barbiturates bind at a beta subunit which is distinct from the benzodiazepine binding site.
Available agents
Mechanism of action
Barbiturates
Although the precise sites of action of barbiturates have not yet been defined, the second and third transmembrane domains of the β subunit appear to be critical; binding may involve a pocket formed by β-subunit methionine 286 as well as α-subunit methionine 236.[9]
Insomnia
Barbiturates were first introduced as hypnotics for patients with schizophrenia. It induced a state of deep and prolonged sleep. But this was not used for long because of adverse effects.[1]
Anticonvulsant
Phenobarbital was the first truly effective drug against epilepsy. It was discovered by accident when given to epileptic patients to help them sleep. The positive side effects were the anticonvulsant properties which reduced the number of seizures and their intensity.[1]
Sedation
Pentobarbital is used as a hypnotic when analgesia is not required. It´s often used in CT imaging when sedation is needed. It is efficient, safe and the recovery time is short.[10] In 2013 the barbiturates Phenobarbital and butabarbital are still used as sedatives in certain cases as well as to antagonize effects of drugs as ephedrine and theophylline. Phenobarbital is used in cases of withdrawal syndromes. It is still used as normal and emergency treatment in some cases of epilepsy.[1]
Benzodiazepine
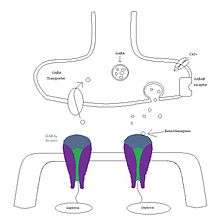
Synaptic action of benzodiazepines: GABAA receptors that are located at synapses are activated when they are exposed to high concentration of GABA. Benzodiazepines enhance the receptor affinity for GABA by decreasing the decay of spontaneous miniature inhibitory postsynaptic currents (mIPSC).[11][12]
Analgesic
Sedative actions of benzodiazepines limit their usefulness as analgesic agents and they are therefore generally not considered to be one but this limitation can be bypassed by intrathecal administration. GABAA receptors in the periaqueductal gray are pro-nociceptive at supraspinal sites while GABAA that are found in the spinal cord are anti-hyperalgesic. Spinal α2 and α3 containing GABAA receptors are the ones responsible for the anti-hyperalgesic action of intrathecal diazepam. This was shown when the anti-hyperalgesic action was reduced when administered in α2 and α3 mice in inflammatory pain and in neuropathic pain. Additionally, studies in α5 mice have shown that the spinal α5-containing GABAA receptor has a minor role in inflammatory pain. An α2, α3 and/or α5 selective positive allosteric agonist, like L-838,427 for example, might be useful as an analgesic drug against inflammatory or neuropathic pain.[2]
Schizophrenia
Benzodiazepines are used as a supporting treatment in patients with schizophrenia.[2]
Depression
GABA ergic hypothesis for depression has been proposed. This hypothesis places the GABA system in a central role in the pathophysiology of depression and in addition to that clinical studies have shown that alprazolam and adinazolam have antidepressant activities in patients with major depressive disorder. Unfortunately we do not know which receptor subtype is responsible for the antidepressant activities. Studies in y2 knockout mice have shown that they display increased anxiety and depressive-like symptoms in despair based tests. The mice also had increased corticosterone concentration which is a symptom in major depression in humans. The y2 subunit is associated with α1-α6 subunits, which are all known α subunits, so these studies do not show which of the α subunits are related to the depressive like symptoms. Other studies with α2 knockout mice have displayed increased anxiety and depression-like symptoms in conflict based feeding tests and the fact that anxiety and depression are often linked seems to indicate that the α2 subunit might be a valid target for a GABAA antidepressant.[2]
Stroke
Preclinical studies have shown that benzodiazepines can be effective in reducing the effect of strokes up to three days after the drug has been administered.[2]
Neurosteroids
Neurosteroids can act as allosteric modulators of neurotransmitter receptors, such as the GABAA,[13][14][15][16] NMDA,[17] and sigma receptors.[18] The neurosteroid Progesterone (PROG) which activates progesterone receptors expressed in peripheral and central glial cells.[19][20][21][22] Additionally it has been surmised that the 3α-hydroxy ring A-reduced pregnane steroids allopregnanolone and tetrahydrodeoxycorticosterone increase the GABA-mediated chloride currents while pregnenolone sulfate and dehydroepiandrosterone (DHEA) sulfate on the other hand have displayed antagonistic properties at the GABAA receptors.
Synthesis
Barbituric acid


Barbituric acid is the parent compound of barbiturate drugs although barbituric acid itself is not pharmacologically active. Barbiturates were synthesized in 1864 by Adolf von Baeyer by combining urea and malonic acid (see figure 5). Synthetic process was later developed and perfected by the French chemist Edouard Grimaux in 1879, making possible the subsequent widespread development of barbiturate derivatives.[23] Malonic acid has since been replaced by diethyl malonate, as using the ester avoids the problem of having to deal with the acidity of the carboxylic acid and its unreactive carboxylate (see figure 6). Barbituric acid can form a large variety of barbiturate drugs by using the Knoevenagel condensation reaction.[24]

Benzodiazepines
The structure that the first benzodiazepine is based on was discovered by Leo H. Sternbach. He thought the compound had a heptoxdiazine structure (See figure 7) but it was later determined to be a quinazoline-3-oxide. Possible drug candidates were then synthesized from that compound and screened for activity. One of these compounds was active, chlordiazepoxide. It was marketed in 1960 and became the first benzodiazepine drug.[25]
Biosynthesis of Neurosteroids
Neurosteroids are synthesized in the central nervous system (CNS) and the peripheral nervous system (PNS) from cholesterol and steroidal precursors that are imported from the peripheral sources. These sources include 3β-hydroxy-Δ5 derivatives, such as pregnenolone (PREG) and dehydroepiandrosterone (DHEA), their sulfates, and reduced metabolites such as the tetrahydro derivative of progesterone 3α-hydroxy-5α-pregnane-20-one (3α,5α-THPROG). After the local synthesis or from metabolism of adrenal of gonadal steroids many neurosteroids accumulate in the brain.[26][27]
Structure-activity relationship
Barbiturates

Some barbiturates have special uses and they are organized into the following 4 classes: ultrashort-, short-, intermediate- and long-acting. Empirically SARs of barbiturants are based on thousands of (animal) tested compounds and they have shown that R and R´ may not be H in position 5 (see figure 8). Also, position 5 confer sedative-hypnotic properties.[10] Generally alkyl branching in position 5 means less lipid solubility and less activity. Unsaturation will show less activity in position 5 and alicyclic and aromatic rings will show less potency. Polar substiuents (-NH2, -OH, -COOH) will decrease lipid solubility but it will also eliminate activity. R´´ in position 1 is usually H but if there is CH3 in that position there is a less lipid solubility and duration. Exchanging S for O atom in position 2 produces thiobarbiturates, which are more lipid-soluble than the oxybarbiturates. In general, the more lipidsoluble the barbiturate, the more rapid its onset, the shorter its duration and the greater the degree of hypnotic activity. Barbiturates have shown some hydrolytic problems in regard to formulation of liquid dosage forms, the difficulty is -OH catalyzed degration of the ureide rings but that can be fixed if the pH is 6 in the formulation. S(-) form of barbiturate have shown more depressant activity while the R(+) isomers have an excitatory effect.[28]
Benzodiazepines

According to a research performed by Maddalena et al. using artificial neural networks position 7 has the most effect on receptor affinity. When the active group in position 7 is made more lipophilic and the electronic charge is increased the receptor affinity increases. In the same study position 2´ was found to be the second most important in affecting the affinity but the group in that position needs to be electrophilic to have an effect. Positions 3, 6’ and 8 are of less importance.[29] If there are made changes to 6, 8, 9 or 4´ the activity is decreased. If the group in position 1 is changed to N-alkyl, haloalkyl, alkynyl and small cycle or aminoalkyl the activity is increased. There can be hydroxylation in position 3 which can cause rapid conjugation and decrease duration and potency (can be clinically useful).[29]

Neurosteroids
In the mid '80s, it was shown for the first time that the neuroactive steroids 3α,5α-tetrahydroprogesterone or allopregnanolone (3α,5α-THP) and 3α,5α-tetrahydrodeoxycorticosterone (3α,5α-THDOC) could modulate neuronal excitability via their interaction with GABAA receptors. The steroids 3α,5α-THP and 3α,5α-THDOC were able not only to displace t-butylbicyclophosphorothionate (TBPS) from the Cl− channel but also to enhance the GABA-elicited Cl− current.[13] In addition, these steroids might enhance the binding of muscimol and benzodiazepines to GABAA receptors.[30] Structure- activity studies (SAR) have shown that the 3alpha-OH group is essential for the anesthetic actions of these steroids,[31] they also have an optimally-placed hydrogen bond accepting group on the β face of the steroid at the C-17 position. The four steroid rings form a rigid framework for positioning these hydrogen groups in three-dimensional space.[32] Analogues 5 and 6 (see figure 10) are weak modulators of GABAA receptor function because the flexible side chains in these analogues do not have the conformations required for high biological activity.[33]
See also
References
- 1 2 3 4 López-Muñoz F, Ucha-Udabe R, Alamo C (Dec 2005). "The history of barbiturates a century after their clinical introduction". Neuropsychiatric Disease and Treatment. 1 (4): 329–43. PMC 2424120
 . PMID 18568113.
. PMID 18568113. - 1 2 3 4 5 Rudolph U, Knoflach F (Sep 2011). "Beyond classical benzodiazepines: novel therapeutic potential of GABAA receptor subtypes". Nature Reviews. Drug Discovery. 10 (9): 685–97. doi:10.1038/nrd3502. PMID 21799515.
- ↑ Lambert JJ, Belelli D, Peden DR, Vardy AW, Peters JA (Sep 2003). "Neurosteroid modulation of GABAA receptors". Progress in Neurobiology. 71 (1): 67–80. doi:10.1016/j.pneurobio.2003.09.001. PMID 14611869.
- ↑ Selye H (1 January 1941). "Anesthetic Effect of Steroid Hormones.". Experimental Biology and Medicine. 46 (1): 116–121. doi:10.3181/00379727-46-11907.
- ↑ Harrison NL, Simmonds MA (Dec 1984). "Modulation of the GABA receptor complex by a steroid anaesthetic". Brain Research. 323 (2): 287–92. doi:10.1016/0006-8993(84)90299-3. PMID 6098342.
- 1 2 Egawa K, Fukuda A (2013). "Pathophysiological power of improper tonic GABA(A) conductances in mature and immature models". Frontiers in Neural Circuits. 7: 170. doi:10.3389/fncir.2013.00170. PMID 24167475.
- ↑ Günther U, Benson J, Benke D, Fritschy JM, Reyes G, Knoflach F, Crestani F, Aguzzi A, Arigoni M, Lang Y (Aug 1995). "Benzodiazepine-insensitive mice generated by targeted disruption of the gamma 2 subunit gene of gamma-aminobutyric acid type A receptors". Proceedings of the National Academy of Sciences of the United States of America. 92 (17): 7749–53. doi:10.1073/pnas.92.17.7749. PMID 7644489.
- ↑ Hosie AM, Wilkins ME, Smart TG (Oct 2007). "Neurosteroid binding sites on GABA(A) receptors". Pharmacology & Therapeutics. 116 (1): 7–19. doi:10.1016/j.pharmthera.2007.03.011. PMID 17560657.
- ↑ Löscher W, Rogawski MA (Dec 2012). "How theories evolved concerning the mechanism of action of barbiturates". Epilepsia. 53 Suppl 8: 12–25. doi:10.1111/epi.12025. PMID 23205959.
- 1 2 Moro-Sutherland DM (September 2000). "Barbiturates". Clinical Pediatric Emergency Medicine. 1 (4): 276–280. doi:10.1016/S1522-8401(00)90040-5.
- ↑ Möhler H, Fritschy JM, Rudolph U (Jan 2002). "A new benzodiazepine pharmacology". The Journal of Pharmacology and Experimental Therapeutics. 300 (1): 2–8. doi:10.1124/jpet.300.1.2. PMID 11752090.
- ↑ Perrais D, Ropert N (Jan 1999). "Effect of zolpidem on miniature IPSCs and occupancy of postsynaptic GABAA receptors in central synapses". The Journal of Neuroscience. 19 (2): 578–88. PMID 9880578.
- 1 2 Majewska MD, Harrison NL, Schwartz RD, Barker JL, Paul SM (May 1986). "Steroid hormone metabolites are barbiturate-like modulators of the GABA receptor". Science. 232 (4753): 1004–7. doi:10.1126/science.2422758. PMID 2422758.
- ↑ Herd MB, Belelli D, Lambert JJ (Oct 2007). "Neurosteroid modulation of synaptic and extrasynaptic GABA(A) receptors". Pharmacology & Therapeutics. 116 (1): 20–34. doi:10.1016/j.pharmthera.2007.03.007. PMID 17531325.
- ↑ Hosie AM, Wilkins ME, da Silva HM, Smart TG (Nov 2006). "Endogenous neurosteroids regulate GABAA receptors through two discrete transmembrane sites". Nature. 444 (7118): 486–9. doi:10.1038/nature05324. PMID 17108970.
- ↑ Puia G, Santi MR, Vicini S, Pritchett DB, Purdy RH, Paul SM, Seeburg PH, Costa E (May 1990). "Neurosteroids act on recombinant human GABAA receptors". Neuron. 4 (5): 759–65. doi:10.1016/0896-6273(90)90202-Q. PMID 2160838.
- ↑ Wu FS, Gibbs TT, Farb DH (Sep 1991). "Pregnenolone sulfate: a positive allosteric modulator at the N-methyl-D-aspartate receptor" (abstract). Molecular Pharmacology. 40 (3): 333–6. PMID 1654510.
- ↑ Maurice T, Junien JL, Privat A (Feb 1997). "Dehydroepiandrosterone sulfate attenuates dizocilpine-induced learning impairment in mice via sigma 1-receptors". Behavioural Brain Research. 83 (1-2): 159–64. doi:10.1016/S0166-4328(97)86061-5. PMID 9062676.
- ↑ Baulieu EE (1997). "Neurosteroids: of the nervous system, by the nervous system, for the nervous system". Recent Progress in Hormone Research. 52: 1–32. PMID 9238846.
- ↑ Rupprecht R, Reul JM, Trapp T, van Steensel B, Wetzel C, Damm K, Zieglgänsberger W, Holsboer F (Sep 1993). "Progesterone receptor-mediated effects of neuroactive steroids". Neuron. 11 (3): 523–30. doi:10.1016/0896-6273(93)90156-L. PMID 8398145.
- ↑ Jung-Testas I, Do Thi A, Koenig H, Désarnaud F, Shazand K, Schumacher M, Baulieu EE (1999). "Progesterone as a neurosteroid: synthesis and actions in rat glial cells". The Journal of Steroid Biochemistry and Molecular Biology. 69 (1-6): 97–107. doi:10.1016/S0960-0760(98)00149-6. PMID 10418983.
- ↑ Belelli D, Lambert JJ (Jul 2005). "Neurosteroids: endogenous regulators of the GABA(A) receptor". Nature Reviews. Neuroscience. 6 (7): 565–75. doi:10.1038/nrn1703. PMID 15959466.
- ↑ Carter, MK (1951). "The history of barbituric acid". J Chem Educ. 28: 525–8. doi:10.1021/ed028p524.
- ↑ Deb ML, Bhuyan, Pulak J. (September 2005). "Uncatalysed Knoevenagel condensation in aqueous medium at room temperature". Tetrahedron Letters. 46 (38): 6453–6456. doi:10.1016/j.tetlet.2005.07.111.
- ↑ Gringauz A (1997). Medicinal Chemistry How drugs act and why. United States of America: WILEY-VCH. pp. 578–579. ISBN 0-471-18545-0.
- ↑ Agís-Balboa RC, Pinna G, Zhubi A, Maloku E, Veldic M, Costa E, Guidotti A (Sep 2006). "Characterization of brain neurons that express enzymes mediating neurosteroid biosynthesis". Proceedings of the National Academy of Sciences of the United States of America. 103 (39): 14602–7. doi:10.1073/pnas.0606544103. PMC 1600006
 . PMID 16984997.
. PMID 16984997. - ↑ Mellon SH, Griffin LD (2002). "Neurosteroids: biochemistry and clinical significance". Trends in Endocrinology and Metabolism. 13 (1): 35–43. doi:10.1016/S1043-2760(01)00503-3. PMID 11750861.
- ↑ Gringauz A (1997). Medicinal Chemistry How drugs act and why. United States of America: Wiley-VCH. pp. 572–574. ISBN 0-471-18545-0.
- 1 2 Maddalena DJ, Johnston GA (Feb 1995). "Prediction of receptor properties and binding affinity of ligands to benzodiazepine/GABAA receptors using artificial neural networks". Journal of Medicinal Chemistry. 38 (4): 715–24. doi:10.1021/jm00004a017. PMID 7861419.
- ↑ Paul SM, Purdy RH (Mar 1992). "Neuroactive steroids". FASEB Journal. 6 (6): 2311–22. PMID 1347506.
- ↑ Covey DF, Han M, Kumar AS, de La Cruz MA, Meadows ES, Hu Y, Tonnies A, Nathan D, Coleman M, Benz A, Evers AS, Zorumski CF, Mennerick S (Aug 2000). "Neurosteroid analogues. 8. Structure-activity studies of N-acylated 17a-aza-D-homosteroid analogues of the anesthetic steroids (3alpha, 5alpha)- and (3alpha,5beta)-3-hydroxypregnan-20-one". Journal of Medicinal Chemistry. 43 (17): 3201–4. doi:10.1021/jm0002477. PMID 10966737.
- ↑ Covey DF, Evers AS, Mennerick S, Zorumski CF, Purdy RH (Nov 2001). "Recent developments in structure-activity relationships for steroid modulators of GABA(A) receptors". Brain Research. Brain Research Reviews. 37 (1-3): 91–7. doi:10.1016/S0165-0173(01)00126-6. PMID 11744077.
- ↑ Covey DF, Hu Y, Bouley MG, Holland KD, Rodgers-Neame NT, Isenberg KE, Zorumski CF (Mar 1993). "Modulation of GABAA receptor function by benz[e]indenes and phenanthrenes". Journal of Medicinal Chemistry. 36 (5): 627–30. doi:10.1021/jm00057a012. PMID 8388475.
Further reading
- Faizi M, Dabirian S, Tajali H, Ahmadi F, Zavareh ER, Shahhosseini S, Tabatabai SA (Feb 2015). "Novel agonists of benzodiazepine receptors: design, synthesis, binding assay and pharmacological evaluation of 1,2,4-triazolo[1,5-a]pyrimidinone and 3-amino-1,2,4-triazole derivatives". Bioorganic & Medicinal Chemistry. 23 (3): 480–7. doi:10.1016/j.bmc.2014.12.016. PMID 25564376.