Medical imaging
| Medical imaging | |
|---|---|
| Diagnostics | |
|
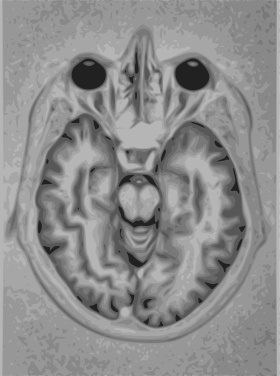
A CT scan image showing a ruptured abdominal aortic aneurysm | |
| ICD-10-PCS | |
| ICD-9 | 87-88 |
| MeSH | D003952 |
| OPS-301 code | 3 |
| MedlinePlus | 007451 |
Medical imaging is the technique and process of creating visual representations of the interior of a body for clinical analysis and medical intervention, as well as visual representation of the function of some organs or tissues (physiology). Medical imaging seeks to reveal internal structures hidden by the skin and bones, as well as to diagnose and treat disease. Medical imaging also establishes a database of normal anatomy and physiology to make it possible to identify abnormalities. Although imaging of removed organs and tissues can be performed for medical reasons, such procedures are usually considered part of pathology instead of medical imaging.
As a discipline and in its widest sense, it is part of biological imaging and incorporates radiology which uses the imaging technologies of X-ray radiography, magnetic resonance imaging, medical ultrasonography or ultrasound, endoscopy, elastography, tactile imaging, thermography, medical photography and nuclear medicine functional imaging techniques as positron emission tomography (PET) and Single-photon emission computed tomography (SPECT).
Measurement and recording techniques which are not primarily designed to produce images, such as electroencephalography (EEG), magnetoencephalography (MEG), electrocardiography (ECG), and others represent other technologies which produce data susceptible to representation as a parameter graph vs. time or maps which contain data about the measurement locations. In a limited comparison these technologies can be considered as forms of medical imaging in another discipline.
Up until 2010, 5 billion medical imaging studies had been conducted worldwide.[1] Radiation exposure from medical imaging in 2006 made up about 50% of total ionizing radiation exposure in the United States.[2]
Medical imaging is often perceived to designate the set of techniques that noninvasively produce images of the internal aspect of the body. In this restricted sense, medical imaging can be seen as the solution of mathematical inverse problems. This means that cause (the properties of living tissue) is inferred from effect (the observed signal). In the case of medical ultrasonography, the probe consists of ultrasonic pressure waves and echoes that go inside the tissue to show the internal structure. In the case of projectional radiography, the probe uses X-ray radiation, which is absorbed at different rates by different tissue types such as bone, muscle and fat.
The term noninvasive is used to denote a procedure where no instrument is introduced into a patient's body which is the case for most imaging techniques used.
Imaging modalities

In the clinical context, "invisible light" medical imaging is generally equated to radiology or "clinical imaging" and the medical practitioner responsible for interpreting (and sometimes acquiring) the images is a radiologist. "Visible light" medical imaging involves digital video or still pictures that can be seen without special equipment. Dermatology and wound care are two modalities that use visible light imagery. Diagnostic radiography designates the technical aspects of medical imaging and in particular the acquisition of medical images. The radiographer or radiologic technologist is usually responsible for acquiring medical images of diagnostic quality, although some radiological interventions are performed by radiologists.
As a field of scientific investigation, medical imaging constitutes a sub-discipline of biomedical engineering, medical physics or medicine depending on the context: Research and development in the area of instrumentation, image acquisition (e.g., radiography), modeling and quantification are usually the preserve of biomedical engineering, medical physics, and computer science; Research into the application and interpretation of medical images is usually the preserve of radiology and the medical sub-discipline relevant to medical condition or area of medical science (neuroscience, cardiology, psychiatry, psychology, etc.) under investigation. Many of the techniques developed for medical imaging also have scientific and industrial applications.[3]
Radiography
Two forms of radiographic images are in use in medical imaging. Projection radiography and fluoroscopy, with the latter being useful for catheter guidance. These 2D techniques are still in wide use despite the advance of 3D tomography due to the low cost, high resolution, and depending on application, lower radiation dosages. This imaging modality utilizes a wide beam of x rays for image acquisition and is the first imaging technique available in modern medicine.
- Fluoroscopy produces real-time images of internal structures of the body in a similar fashion to radiography, but employs a constant input of x-rays, at a lower dose rate. Contrast media, such as barium, iodine, and air are used to visualize internal organs as they work. Fluoroscopy is also used in image-guided procedures when constant feedback during a procedure is required. An image receptor is required to convert the radiation into an image after it has passed through the area of interest. Early on this was a fluorescing screen, which gave way to an Image Amplifier (IA) which was a large vacuum tube that had the receiving end coated with cesium iodide, and a mirror at the opposite end. Eventually the mirror was replaced with a TV camera.
- Projectional radiographs, more commonly known as x-rays, are often used to determine the type and extent of a fracture as well as for detecting pathological changes in the lungs. With the use of radio-opaque contrast media, such as barium, they can also be used to visualize the structure of the stomach and intestines - this can help diagnose ulcers or certain types of colon cancer.
Magnetic Resonance Imaging (MRI)
A magnetic resonance imaging instrument (MRI scanner), or "nuclear magnetic resonance (NMR) imaging" scanner as it was originally known, uses powerful magnets to polarize and excite hydrogen nuclei (i.e., single protons) of water molecules in human tissue, producing a detectable signal which is spatially encoded, resulting in images of the body.[4] The MRI machine emits a radio frequency (RF) pulse at the resonant frequency of the hydrogen atoms on water molecules. Radio frequency antennas ("RF coils") send the pulse to the area of the body to be examined. The RF pulse is absorbed by protons, causing their direction with respect to the primary magnetic field to change. When the RF pulse is turned off, the protons "relax" back to alignment with the primary magnet and emit radio-waves in the process. This radio-frequency emission from the hydrogen-atoms on water is what is detected and reconstructed into an image. The resonant frequency of a spinning magnetic dipole (of which protons are one example) is called the Larmor frequency and is determined by the strength of the main magnetic field and the chemical environment of the nuclei of interest. MRI uses three electromagnetic fields: a very strong (typically 1.5 to 3 teslas) static magnetic field to polarize the hydrogen nuclei, called the primary field; gradient fields that can be modified to vary in space and time (on the order of 1 kHz) for spatial encoding, often simply called gradients; and a spatially homogeneous radio-frequency (RF) field for manipulation of the hydrogen nuclei to produce measurable signals, collected through an RF antenna.
Like CT, MRI traditionally creates a two dimensional image of a thin "slice" of the body and is therefore considered a tomographic imaging technique. Modern MRI instruments are capable of producing images in the form of 3D blocks, which may be considered a generalization of the single-slice, tomographic, concept. Unlike CT, MRI does not involve the use of ionizing radiation and is therefore not associated with the same health hazards. For example, because MRI has only been in use since the early 1980s, there are no known long-term effects of exposure to strong static fields (this is the subject of some debate; see 'Safety' in MRI) and therefore there is no limit to the number of scans to which an individual can be subjected, in contrast with X-ray and CT. However, there are well-identified health risks associated with tissue heating from exposure to the RF field and the presence of implanted devices in the body, such as pace makers. These risks are strictly controlled as part of the design of the instrument and the scanning protocols used.
Because CT and MRI are sensitive to different tissue properties, the appearance of the images obtained with the two techniques differ markedly. In CT, X-rays must be blocked by some form of dense tissue to create an image, so the image quality when looking at soft tissues will be poor. In MRI, while any nucleus with a net nuclear spin can be used, the proton of the hydrogen atom remains the most widely used, especially in the clinical setting, because it is so ubiquitous and returns a large signal. This nucleus, present in water molecules, allows the excellent soft-tissue contrast achievable with MRI.
A number of different pulse sequences can be used for specific MRI diagnostic imaging (multiparametric MRI or mpMRI). It is possible to differentiate tissue characteristics by combining two or more of the following imaging sequences, depending on the information being sought: T1-weighted (T1-MRI), T2-weighted (T2-MRI), diffusion weighted imaging (DWI-MRI), dynamic contrast enhancement (DCE-MRI), and spectroscopy (MRI-S). For example, imaging of prostate tumors is better accomplished using T2-MRI and DWI-MRI than T2-weighted imaging alone.[5] The number of applications of mpMRI for detecting disease in various organs continues to expand, including liver studies, breast tumors, pancreatic tumors, and assessing the effects of vascular disruption agents on cancer tumors.[6][7][8]
Nuclear medicine
Nuclear medicine encompasses both diagnostic imaging and treatment of disease, and may also be referred to as molecular medicine or molecular imaging & therapeutics.[9] Nuclear medicine uses certain properties of isotopes and the energetic particles emitted from radioactive material to diagnose or treat various pathology. Different from the typical concept of anatomic radiology, nuclear medicine enables assessment of physiology. This function-based approach to medical evaluation has useful applications in most subspecialties, notably oncology, neurology, and cardiology. Gamma cameras and PET scanners are used in e.g. scintigraphy, SPECT and PET to detect regions of biologic activity that may be associated with disease. Relatively short lived isotope, such as 99mTc is administered to the patient. Isotopes are often preferentially absorbed by biologically active tissue in the body, and can be used to identify tumors or fracture points in bone. Images are acquired after collimated photons are detected by a crystal that gives off a light signal, which is in turn amplified and converted into count data.
- Scintigraphy ("scint") is a form of diagnostic test wherein radioisotopes are taken internally, for example intravenously or orally. Then, gamma cameras capture and form two-dimensional[10] images from the radiation emitted by the radiopharmaceuticals.
- SPECT is a 3D tomographic technique that uses gamma camera data from many projections and can be reconstructed in different planes. A dual detector head gamma camera combined with a CT scanner, which provides localization of functional SPECT data, is termed a SPECT-CT camera, and has shown utility in advancing the field of molecular imaging. In most other medical imaging modalities, energy is passed through the body and the reaction or result is read by detectors. In SPECT imaging, the patient is injected with a radioisotope, most commonly Thallium 201TI, Technetium 99mTC, Iodine 123I, and Gallium 67Ga.[11] The radioactive gamma rays are emitted through the body as the natural decaying process of these isotopes takes place. The emissions of the gamma rays are captured by detectors that surround the body. This essentially means that the human is now the source of the radioactivity, rather than the medical imaging devices such as X-Ray or CT.
- Positron emission tomography (PET) uses coincidence detection to image functional processes. Short-lived positron emitting isotope, such as 18F, is incorporated with an organic substance such as glucose, creating F18-fluorodeoxyglucose, which can be used as a marker of metabolic utilization. Images of activity distribution throughout the body can show rapidly growing tissue, like tumor, metastasis, or infection. PET images can be viewed in comparison to computed tomography scans to determine an anatomic correlate. Modern scanners may integrate PET, allowing PET-CT, or PET-MRI to optimize the image reconstruction involved with positron imaging. This is performed on the same equipment without physically moving the patient off of the gantry. The resultant hybrid of functional and anatomic imaging information is a useful tool in non-invasive diagnosis and patient management.
Fiduciary markers are used in a wide range of medical imaging applications. Images of the same subject produced with two different imaging systems may be correlated (called image registration) by placing a fiduciary marker in the area imaged by both systems. In this case, a marker which is visible in the images produced by both imaging modalities must be used. By this method, functional information from SPECT or positron emission tomography can be related to anatomical information provided by magnetic resonance imaging (MRI).[12] Similarly, fiducial points established during MRI can be correlated with brain images generated by magnetoencephalography to localize the source of brain activity.

Ultrasound
Medical ultrasonography uses high frequency broadband sound waves in the megahertz range that are reflected by tissue to varying degrees to produce (up to 3D) images. This is commonly associated with imaging the fetus in pregnant women. Uses of ultrasound are much broader, however. Other important uses include imaging the abdominal organs, heart, breast, muscles, tendons, arteries and veins. While it may provide less anatomical detail than techniques such as CT or MRI, it has several advantages which make it ideal in numerous situations, in particular that it studies the function of moving structures in real-time, emits no ionizing radiation, and contains speckle that can be used in elastography. Ultrasound is also used as a popular research tool for capturing raw data, that can be made available through an ultrasound research interface, for the purpose of tissue characterization and implementation of new image processing techniques. The concepts of ultrasound differ from other medical imaging modalities in the fact that it is operated by the transmission and receipt of sound waves. The high frequency sound waves are sent into the tissue and depending on the composition of the different tissues; the signal will be attenuated and returned at separate intervals. A path of reflected sound waves in a multilayered structure can be defined by an input acoustic impedance (ultrasound sound wave) and the Reflection and transmission coefficients of the relative structures.[11] It is very safe to use and does not appear to cause any adverse effects. It is also relatively inexpensive and quick to perform. Ultrasound scanners can be taken to critically ill patients in intensive care units, avoiding the danger caused while moving the patient to the radiology department. The real time moving image obtained can be used to guide drainage and biopsy procedures. Doppler capabilities on modern scanners allow the blood flow in arteries and veins to be assessed.
Elastography
Elastography is a relatively new imaging modality that maps the elastic properties of soft tissue. This modality emerged in the last two decades. Elastography is useful in medical diagnoses, as elasticity can discern healthy from unhealthy tissue for specific organs/growths. For example, cancerous tumours will often be harder than the surrounding tissue, and diseased livers are stiffer than healthy ones.[13][14][15][16] There are a several elastographic techniques based on the use of ultrasound, magnetic resonance imaging and tactile imaging. The wide clinical use of ultrasound elastography is a result of the implementation of technology in clinical ultrasound machines. Main branches of ultrasound elastography include Quasistatic Elastography/Strain Imaging, Shear Wave Elasticity Imaging (SWEI), Acoustic Radiation Force Impulse imaging (ARFI), Supersonic Shear Imaging (SSI), and Transient Elastography.[14] In the last decade a steady increase of activities in the field of elastography is observed demonstrating successful application of the technology in various areas of medical diagnostics and treatment monitoring.

Tactile imaging
Tactile imaging is a medical imaging modality that translates the sense of touch into a digital image. The tactile image is a function of P(x,y,z), where P is the pressure on soft tissue surface under applied deformation and x,y,z are coordinates where pressure P was measured. Tactile imaging closely mimics manual palpation, since the probe of the device with a pressure sensor array mounted on its face acts similar to human fingers during clinical examination, slightly deforming soft tissue by the probe and detecting resulting changes in the pressure pattern. Figure on the right presents an experiment on a composite tissue phantom examined by a tactile imaging probe illustrating the ability of tactile imaging to visualize in 3D the structure of the object.
This modality is used for imaging of the prostate,[17] breast,[18] vagina and pelvic floor support structures,[19] and myofascial trigger points in muscle.[20]
Photoacoustic imaging
Photoacoustic imaging is a recently developed hybrid biomedical imaging modality based on the photoacoustic effect. It combines the advantages of optical absorption contrast with ultrasonic spatial resolution for deep imaging in (optical) diffusive or quasi-diffusive regime. Recent studies have shown that photoacoustic imaging can be used in vivo for tumor angiogenesis monitoring, blood oxygenation mapping, functional brain imaging, and skin melanoma detection, etc.
Thermography
Primarily used for breast imaging. There are three approaches: tele-thermography, contact thermography and dynamic angiothermography. These digital infrared imaging thermographic techniques are based on the principle that metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in normal breast tissue. Cancerous tumors require an ever-increasing supply of nutrients and therefore increase circulation to their cells by holding open existing blood vessels, opening dormant vessels, and creating new ones (neo-angiogenesis theory).
Tele-thermography and contact thermography supporters claim this process results in an increase in regional surface temperatures of the breast, however there is little evidence that thermography is an accurate means of identifying breast tumours. Thermography is not approved for breast cancer screening in the United States or Canada, and medical authorities have issued warnings against thermography in both countries.[21]
Dynamic angiothermography utilizes thermal imaging but with important differences with the tele-thermography and contact thermography, that impact detection performance. First, the probes are improved over the previous liquid crystal plates; they include better spatial resolution, contrastive performance, and the image is formed more quickly. The more significant difference[22] lies in identifying the thermal changes due to changes in vascular network to support the growth of the tumor/lesion. Instead of just recording the change in heat generated by the tumor, the image is now able to identify changes due to the vascularization of the mammary gland. It is currently used in combination with other techniques for diagnosis of breast cancer. This diagnostic method is a low cost one compared with other techniques. The angiothermography is not a test that substitutes for other tests, but stands in relation to them as a technique that gives additional information to clarify the clinical picture and improve the quality of diagnosis.
Tomography
Tomography is the method of imaging a single plane, or slice, of an object resulting in a tomogram. There are two principal methods of obtaining such images, conventional and computer-assisted tomography. Conventional tomography uses mechanical means to record an image directly onto X-ray film, while in computer-assisted tomography, a computer processes information fed to it from detectors then constructs a virtual image which can be stored in digital format and can be displayed on a screen, or printed on paper or film.
Conventional tomography
In conventional tomography, mechanical movement of an X-ray source and film in unison generates a tomogram using the principles of projective geometry.[23] Synchronizing the movement of the radiation source and detector which are situated in the opposite direction from each other causes structures which are not in the focal plane being studied to blur out. This was the main method of obtaining tomographic images until the late-1970s. It is now considered obsolete (except for certain dental applications), having been replaced with computer-assisted tomographic techniques. Historically, there have been various techniques involved in conventional tomography:
- Linear tomography: This is the most basic form of conventional tomography. The X-ray tube moved from point "A" to point "B" above the patient, while the cassette holder (or "bucky") moves simultaneously under the patient from point "B" to point "A." The fulcrum, or pivot point, is set to the area of interest. In this manner, the points above and below the focal plane are blurred out, just as the background is blurred when panning a camera during exposure. Rarely used, and has largely been replaced by computed tomography (CT).
- Poly tomography: This was achieved using a more advanced X-ray apparatus that allows for more sophisticated and continuous movements of the X-ray tube and film. With this technique, a number of complex synchronous geometrical movements could be programmed, such as hypocycloidic, circular, figure 8, and elliptical. Philips Medical Systems for example produced one such device called the 'Polytome'.[23] This pluridirectional unit was still in use into the 1990s, as its resulting images for small or difficult physiology, such as the inner ear, was still difficult to image with CTs at that time. As the resolution of CTs got better, this procedure was taken over by CT.
- Zonography: This is a variant of linear tomography, where a limited arc of movement is used. It is still used in some centres for visualising the kidney during an intravenous urogram (IVU), though it too is being supplanted by CT.
- Panoramic radiograph: The only common tomographic examination still in use. This makes use of a complex movement to allow the radiographic examination of the mandible, as if it were a flat bone. It is commonly performed in dental practices and is often referred to as a "Panorex", but this is incorrect, as it is a trademark of a specific company.
Computer-assisted tomography
In computer-assisted tomography, a computer processes data received from radiation detectors and computationally constructs an image of the structures being scanned. Imaging techniques using this method are far superior to conventional tomography as they can readily image both soft and hard tissues (while conventional tomography is quite poor at imaging soft tissues). The following techniques exist:
- X-ray computed tomography (CT), or Computed Axial Tomography (CAT) scan, is a helical tomography technique (latest generation), which traditionally produces a 2D image of the structures in a thin section of the body. In CT, a beam of X-rays spins around an object being examined and is picked up by sensitive radiation detectors after having penetrated the object from multiple angles. A computer then analyses the information received from the scanner's detectors and constructs a detailed image of the object and its contents using the mathematical principles laid out in the Radon transform. It has a greater ionizing radiation dose burden than projection radiography; repeated scans must be limited to avoid health effects. CT is based on the same principles as X-Ray projections but in this case, the patient is enclosed in a surrounding ring of detectors assigned with 500-1000 scintillation detectors[11] (fourth-generation X-Ray CT scanner geometry). Previously in older generation scanners, the X-Ray beam was paired by a translating source and detector.
- Positron emission tomography (PET) also used in conjunction with computed tomography, PET-CT, and magnetic resonance imaging PET-MRI.
- Magnetic resonance imaging (MRI) commonly produces tomographic images of cross-sections of the body. (See separate MRI section in this article.)
Echocardiography
When ultrasound is used to image the heart it is referred to as an echocardiogram. Echocardiography allows detailed structures of the heart, including chamber size, heart function, the valves of the heart, as well as the pericardium (the sac around the heart) to be seen. Echocardiography uses 2D, 3D, and Doppler imaging to create pictures of the heart and visualize the blood flowing through each of the four heart valves. Echocardiography is widely used in an array of patients ranging from those experiencing symptoms, such as shortness of breath or chest pain, to those undergoing cancer treatments. Transthoracic ultrasound has been proven to be safe for patients of all ages, from infants to the elderly, without risk of harmful side effects or radiation, differentiating it from other imaging modalities. Echocardiography is one of the most commonly used imaging modalities in the world due to its portability and use in a variety of applications. In emergency situations, echocardiography is quick, easily accessible, and able to be performed at the bedside, making it the modality of choice for many physicians.
Functional near-infrared spectroscopy
FNIR Is a relatively new non-invasive imaging technique. NIRS (near infrared spectroscopy) is used for the purpose of functional neuroimaging and has been widely accepted as a brain imaging technique.[24]
Medical imaging topics
Image Gently and Image Wisely Campaigns
In response to increased concern by the public over radiation doses and the ongoing progress of best practices, The Alliance for Radiation Safety in Pediatric Imaging was formed within the Society for Pediatric Radiology. In concert with The American Society of Radiologic Technologists, The American College of Radiology and The American Association of Physicists in Medicine, the Society for Pediatric Radiology developed and launched the Image Gently Campaign which is designed to maintain high quality imaging studies while using the lowest doses and best radiation safety practices available on pediatric patients.[25] This initiative has been endorsed and applied by a growing list of various Professional Medical organizations around the world and has received support and assistance from companies that manufacture equipment used in Radiology.
Following upon the success of the Image Gently campaign, the American College of Radiology, the Radiological Society of North America, the American Association of Physicists in Medicine and the American Society of Radiologic Technologists have launched a similar campaign to address this issue in the adult population called Image Wisely.[26] The World Health Organization and International Atomic Energy Agency (IAEA) of the United Nations have also been working in this area and have ongoing projects designed to broaden best practices and lower patient radiation dose.[27][28][29]
DICOM
The Digital Imaging and Communication in Medicine (DICOM) Standard is used globally to store, exchange, and transmit medical images. The DICOM Standard incorporates protocols for imaging techniques such as radiography, computed tomography (CT), magnetic resonance imaging (MRI), ultrasonography, and radiation therapy.[30] DICOM includes standards for image exchange (e.g., via portable media such as DVDs), image compression, 3-D visualization, image presentation, and results reporting.[31]
Maximizing imaging procedure use
The amount of data obtained in a single MR or CT scan is very extensive. Some of the data that radiologists discard could save patients time and money, while reducing their exposure to radiation and risk of complications from invasive procedures.[32] Another approach for making the procedures more efficient is based on utilizing additional constraints, e.g., in some medical imaging modalities one can improve the efficiency of the data acquisition by taking into account the fact the reconstructed density is positive.[33]
Creation of three-dimensional images
Recently, techniques have been developed to enable CT, MRI and ultrasound scanning software to produce 3D images for the physician.[34] Traditionally CT and MRI scans produced 2D static output on film. To produce 3D images, many scans are made, then combined by computers to produce a 3D model, which can then be manipulated by the physician. 3D ultrasounds are produced using a somewhat similar technique. In diagnosing disease of the viscera of abdomen, ultrasound is particularly sensitive on imaging of biliary tract, urinary tract and female reproductive organs (ovary, fallopian tubes). As for example, diagnosis of gall stone by dilatation of common bile duct and stone in common bile duct. With the ability to visualize important structures in great detail, 3D visualization methods are a valuable resource for the diagnosis and surgical treatment of many pathologies. It was a key resource for the famous, but ultimately unsuccessful attempt by Singaporean surgeons to separate Iranian twins Ladan and Laleh Bijani in 2003. The 3D equipment was used previously for similar operations with great success.
Other proposed or developed techniques include:
- Diffuse optical tomography
- Elastography
- Electrical impedance tomography
- Optoacoustic imaging
- Ophthalmology
Some of these techniques are still at a research stage and not yet used in clinical routines.
Compression of medical images
Medical imaging techniques produce very large amounts of data, especially from CT, MRI and PET modalities. As a result, storage and communications of electronic image data are prohibitive without the use of compression. JPEG 2000 is the state-of-the-art image compression DICOM standard for storage and transmission of medical images. The cost and feasibility of accessing large image data sets over low or various bandwidths are further addressed by use of another DICOM standard, called JPIP, to enable efficient streaming of the JPEG 2000 compressed image data.
Non-diagnostic imaging
Neuroimaging has also been used in experimental circumstances to allow people (especially disabled persons) to control outside devices, acting as a brain computer interface.
Many medical imaging software applications (3DSlicer, ImageJ, MIPAV , etc.) are used for non-diagnostic imaging, specifically because they don't have an FDA approval[35] and not allowed to use in clinical research for patient diagnosis.[36] Note that many clinical research studies are not designed for patient diagnosis anyway.[37]
Archiving and recording
Used primarily in ultrasound imaging, capturing the image produced by a medical imaging device is required for archiving and telemedicine applications. In most scenarios, a frame grabber is used in order to capture the video signal from the medical device and relay it to a computer for further processing and operations.[38]
Medical Imaging in the Cloud
There has been growing trend to migrate from PACS to a Cloud Based RIS. A recent article by Applied Radiology said, "As the digital-imaging realm is embraced across the healthcare enterprise, the swift transition from terabytes to petabytes of data has put radiology on the brink of information overload. Cloud computing offers the imaging department of the future the tools to manage data much more intelligently."[39]
Use in pharmaceutical clinical trials
Medical imaging has become a major tool in clinical trials since it enables rapid diagnosis with visualization and quantitative assessment.
A typical clinical trial goes through multiple phases and can take up to eight years. Clinical endpoints or outcomes are used to determine whether the therapy is safe and effective. Once a patient reaches the endpoint, he or she is generally excluded from further experimental interaction. Trials that rely solely on clinical endpoints are very costly as they have long durations and tend to need large numbers of patients.
In contrast to clinical endpoints, surrogate endpoints have been shown to cut down the time required to confirm whether a drug has clinical benefits. Imaging biomarkers (a characteristic that is objectively measured by an imaging technique, which is used as an indicator of pharmacological response to a therapy) and surrogate endpoints have shown to facilitate the use of small group sizes, obtaining quick results with good statistical power.[40]
Imaging is able to reveal subtle change that is indicative of the progression of therapy that may be missed out by more subjective, traditional approaches. Statistical bias is reduced as the findings are evaluated without any direct patient contact.
Imaging techniques such as positron emission tomography (PET) and magnetic resonance imaging (MRI) are routinely used in oncology and neuroscience areas,.[41][42][43][44] For example, measurement of tumour shrinkage is a commonly used surrogate endpoint in solid tumour response evaluation. This allows for faster and more objective assessment of the effects of anticancer drugs. In Alzheimer's disease, MRI scans of the entire brain can accurately assess the rate of hippocampal atrophy, while PET scans can measure the brain's metabolic activity by measuring regional glucose metabolism,[40] and beta-amyloid plaques using tracers such as Pittsburgh compound B (PiB). Historically less use has been made of quantitative medical imaging in other areas of drug development although interest is growing.[45]
An imaging-based trial will usually be made up of three components:
- A realistic imaging protocol. The protocol is an outline that standardizes (as far as practically possible) the way in which the images are acquired using the various modalities (PET, SPECT, CT, MRI). It covers the specifics in which images are to be stored, processed and evaluated.
- An imaging centre that is responsible for collecting the images, perform quality control and provide tools for data storage, distribution and analysis. It is important for images acquired at different time points are displayed in a standardised format to maintain the reliability of the evaluation. Certain specialised imaging contract research organizations provide end to end medical imaging services, from protocol design and site management through to data quality assurance and image analysis.
- Clinical sites that recruit patients to generate the images to send back to the imaging centre.
Shielding
| X-rays generated by peak voltages below | Minimum thickness of lead |
|---|---|
| 75 kV | 1.0 mm |
| 100 kV | 1.5 mm |
| 125 kV | 2.0 mm |
| 150 kV | 2.5 mm |
| 175 kV | 3.0 mm |
| 200 kV | 4.0 mm |
| 225 kV | 5.0 mm |
| 300 kV | 9.0 mm |
| 400 kV | 15.0 mm |
| 500 kV | 22.0 mm |
| 600 kV | 34.0 mm |
| 900 kV | 51.0 mm |
Lead is the most common shield against X-rays because of its high density (11340 kg/m3), stopping power, ease of installation and low cost. The maximum range of a high-energy photon such as an X-ray in matter is infinite; at every point in the matter traversed by the photon, there is a probability of interaction. Thus there is a very small probability of no interaction over very large distances. The shielding of photon beam is therefore exponential (with an attenuation length being close to the radiation length of the material); doubling the thickness of shielding will square the shielding effect.
The following table shows the recommended thickness of lead shielding in function of X-ray energy, from the Recommendations by the Second International Congress of Radiology.[46]
Further reading
- A good comprehensive Medical Imaging Textbook albeit a bit dated: Cho, Zang-Hee, Joie P. Jones, and Manbir Singh. Foundations of medical imaging. New York:: Wiley, 1993.[47]
- Eisenberg, Ronald L.; Margulis, Alexander R.: A Patient's Guide to Medical Imaging. Oxford University Press, 2011. ISBN 978-0-19-972991-3
<!—PLEASE RESPECT ALPHABETICAL ORDER--> Jayaram K. Udupa, Gabor T. Herman “3D Imaging in Medicine, Second Edition” 2nd September 28, 1999 by CRC Press Reference - 384 Pages ISBN 9780849331794 - CAT# 3179 Provides over 100 color images that effectively portray details, particularly for 3D renditions. http://www.mipg.upenn.edu
References
- ↑ Roobottom CA, Mitchell G, Morgan-Hughes G; Mitchell; Morgan-Hughes (November 2010). "Radiation-reduction strategies in cardiac computed tomographic angiography". Clin Radiol. 65 (11): 859–67. doi:10.1016/j.crad.2010.04.021. PMID 20933639.
- ↑ "Medical Radiation Exposure Of The U.S. Population Greatly Increased Since The Early 1980s".
- 1 2 James A.P.; Dasarathy B V. "Medical Image Fusion: A survey of state of the art". Information Fusion. 19: 4–19. doi:10.1016/j.inffus.2013.12.002.
- ↑ "An introduction to magnetic resonance imaging". 2014.
- ↑ Sperling, MD, D. "Combining MRI parameters is better than T2 weighting alone". sperlingprostatecenter.com. Sperling Prostate Center. Retrieved 31 March 2016.
- ↑ Banerjee, Rajarshi; Pavlides, Michael; Tunnicliffe, Elizabeth M.; Piechnik, Stefan K.; Sarania, Nikita; Philips, Rachel; Collier, Jane D.; Booth, Jonathan C.; Schneider, Jurgen E.; Wang, Lai Mun; Delaney, David W.; Fleming, Ken A.; Robson, Matthew D.; Barnes, Eleanor; Neubauer, Stefan (January 2014). "Multiparametric magnetic resonance for the non-invasive diagnosis of liver disease". Journal of Hepatology. 60 (1): 69–77. doi:10.1016/j.jhep.2013.09.002.
- ↑ Rahbar, Habib; Partridge, Savannah C. (February 2016). "Multiparametric MR Imaging of Breast Cancer". Magnetic Resonance Imaging Clinics of North America. 24 (1): 223–238. doi:10.1016/j.mric.2015.08.012.
- ↑ Scialpi, Michele; Reginelli, Alfonso; D'Andrea, Alfredo; Gravante, Sabrina; Falcone, Giuseppe; Baccari, Paolo; Manganaro, Lucia; Palumbo, Barbara; Cappabianca, Salvatore (January 2016). "Pancreatic tumors imaging: An update". International Journal of Surgery. 28: S142–S155. doi:10.1016/j.ijsu.2015.12.053.
- ↑ "Society of Nuclear Medicine and Molecular Imaging (SNMMI)". Snm.org. Retrieved 2013-08-16.
- ↑ "scintigraphy - definition of scintigraphy in the Medical dictionary - by the Free Online Medical Dictionary, Thesaurus and Encyclopedia". Medical-dictionary.thefreedictionary.com. Retrieved 2013-08-16.
- 1 2 3 Dhawan P, A. (2003). Medical Imaging Analysis. Hoboken, NJ: Wiley-Interscience Publication
- ↑ BJ Erickson; CR Jack Jr. "Correlation of single photon emission CT with MR image data using fiduciary markers". American Journal of Neuroradiology, Vol 14, Issue 3 713-720.
- ↑ Wells P. N. T. (2011). "Medical ultrasound: imaging of soft tissue strain and elasticity". Journal of the Royal Society, Interface. 8 (64): 1521–1549. doi:10.1098/rsif.2011.0054.
- 1 2 Sarvazyan A, Hall TJ, Urban MW, Fatemi M, Aglyamov SR, Garra BS (2011). "Overview of elastography–an emerging branch of medical imaging". Current Medical Imaging Reviews. 7 (4): 255–282. doi:10.2174/157340511798038684. PMC 3269947
 . PMID 22308105.
. PMID 22308105. - ↑ Ophir J.; Céspides I.; Ponnekanti H.; Li X. (1991). "Elastography: A quantitative method for imaging the elasticity of biological tissues". Ultrasonic Imaging. 13 (2): 111–134. doi:10.1016/0161-7346(91)90079-W.
- ↑ Parker KJ, Doyley MM, Rubens DJ (2011). "Imaging the elastic properties of tissue: the 20 year perspective". Physics in Medicine and Biology. 56 (2): 513. doi:10.1088/0031-9155/57/16/5359.
- ↑ Weiss RE, Egorov V, Ayrapetyan S, Sarvazyan N, Sarvazyan A (2008). "Prostate mechanical imaging: a new method for prostate assessment". Urology. 71 (3): 425–429. doi:10.1016/j.urology.2007.11.021. PMC 2323601
 . PMID 18342178.
. PMID 18342178. - ↑ Egorov, V.; Sarvazyan, A. P. (2008). "Mechanical Imaging of the Breast". IEEE Transactions on Medical Imaging. 27 (9): 1275–1287. doi:10.1109/TMI.2008.922192. PMC 2581459
 . PMID 18753043.
. PMID 18753043. - ↑ Egorov, V.; Van Raalte, H.; Sarvazyan, A. P. (2010). "Vaginal Tactile Imaging". IEEE Transactions on Biomedical Engineering. 57 (7): 1736–1744. doi:10.1109/TBME.2010.2045757. PMC 3079341
 . PMID 20483695.
. PMID 20483695. - ↑ Turo D, Otto P, Egorov V, Sarvazyan A, Gerber LH, Sikdar S (2012). "Elastography and tactile imaging for mechanical characterization of superficial muscles". J Acoust Soc Am. 132 (3): 1983. doi:10.1121/1.4755316.
- ↑ CBC News. "Health Canada issues advisory about thermography tests". Retrieved 1 December 2012.
- ↑ A new type of breast contact thermography plate: a preliminary and qualitative investigation of its potentiality on phantoms, Montruccoli GC, Montruccoli Salmi D, Casali F, Physica Medica, Vol. XX, N.1, January–March 2004 pp. 27–31.
- 1 2 Littleton, J.T. "Conventional Tomography". A History of the Radiological Sciences (PDF). American Roentgen Ray Society. Retrieved 11 January 2014.
- ↑ Villringer A., Chance B.; Chance (1997). "Non-invasive optical spectroscopy and imaging of human brain function". Trends in Neurosciences. 20 (10): 435–442. doi:10.1016/s0166-2236(97)01132-6. PMID 9347608.
- ↑ "IG new: The Alliance | image gently". Pedrad.org. Retrieved 2013-08-16.
- ↑ "Radiation Safety in Adult Medical Imaging". Image Wisely. Retrieved 2013-08-16.
- ↑ "Optimal levels of radiation for patients - Pan American Health Organization - Organización Panamericana de la Salud". New.paho.org. 2010-08-24. Retrieved 2013-08-16.
- ↑ "Radiation Protection of Patients". Rpop.iaea.org. 2013-03-14. Retrieved 2013-08-16.
- ↑ "World Health Organisation: Global Initiative on Radiation Safety in Healthcare Settings: Technical Meeting Report" (PDF). Who.int. Retrieved 2013-08-16.
- ↑ Kahn, Charles E.; Carrino, John A.; Flynn, Michael J.; Peck, Donald J.; Horii, Steven C. (2007-09-01). "DICOM and Radiology: Past, Present, and Future". Journal of the American College of Radiology. 4 (9): 652–657. doi:10.1016/j.jacr.2007.06.004. ISSN 1546-1440.
- ↑ "DICOM Homepage". dicom.nema.org. Retrieved 2016-05-24.
- ↑ Freiherr G. Waste not, want not: Getting the most from imaging procedures. Diagnostic Imaging. March 19, 2010.
- ↑ Nemirovsky, Jonathan; Shimron, Efrat (2015). "Utilizing Bochners Theorem for Constrained Evaluation of Missing Fourier Data". arXiv:1506.03300
 [physics.med-ph].
[physics.med-ph]. - ↑ Udupa, J.K. and Herman, G. T., 3D Imaging in Medicine, 2nd Edition, CRC Press, 2000
- ↑ FDA: Device Approvals and Clearances, - . Retrieved 2012-31-08
- ↑ "FDA: Statistical Guidance for Clinical Trials of Non Diagnostic Medical Devices". Fda.gov. Retrieved August 31, 2012.
- ↑ Kolata, Gina (August 25, 2012). "Genes Now Tell Doctors Secrets They Can't Utter". The New York Times. Retrieved August 31, 2012.
- ↑ "Treating Medical Ailments in Real Time Using Epiphan DVI2USB | Solutions | Epiphan Systems". Epiphan.com. Retrieved 2013-08-16.
- ↑ Applied Radiology : Imaging on the Cloud : Series=Vol 40, Number 05, May 2011: Rasu B. Shrestha, MD, MBA
- 1 2 Hajnal, J. V., Hawkes, D. J., & Hill, D. L. (2001). Medical Image Registration. CRC Press.
- ↑ Hargreaves, RJ (February 2008). "The role of molecular imaging in drug discovery and development.". Clinical pharmacology and therapeutics. 83 (2): 349–53. doi:10.1038/sj.clpt.6100467. PMID 18167503.
- ↑ Willmann, JK; van Bruggen, N; Dinkelborg, LM; Gambhir, SS (July 2008). "Molecular imaging in drug development". Nature Reviews Drug Discovery. 7 (7): 591–607. doi:10.1038/nrd2290. PMID 18591980.
- ↑ McCarthy, TJ (August 2009). "The role of imaging in drug development.". The quarterly journal of nuclear medicine and molecular imaging : official publication of the Italian Association of Nuclear Medicine (AIMN) [and] the International Association of Radiopharmacology (IAR), [and] Section of the Society of ... 53 (4): 382–6. PMID 19834447.
- ↑ Matthews, PM; Rabiner, I; Gunn, R (October 2011). "Non-invasive imaging in experimental medicine for drug development.". Current Opinion in Pharmacology. 11 (5): 501–7. doi:10.1016/j.coph.2011.04.009. PMID 21570913.
- ↑ Comley, RA; Kallend, D (February 2013). "Imaging in the cardiovascular and metabolic disease area". Drug Discovery Today. 18 (3–4): 185–92. doi:10.1016/j.drudis.2012.09.008. PMID 23032726.
- ↑ Alchemy Art Lead Products – Lead Shielding Sheet Lead For Shielding Applications. Retrieved 2008-12-07.
- ↑ Singh, Z.H. Cho ; Joie P. Jones ; Manbir (1993). Foundations of medical imaging ([Nachdr.]. ed.). New York [u.a.]: Wiley. ISBN 0-471-54573-2.
External links
| Wikimedia Commons has media related to Medical imaging. |
Oldest Medical Imaging Group UPenn Medical Imaging Processing Group, MIPG
- Medical imaging at DMOZ
- MedPix Free Medical Image Database, Search & Download Images
- IPRG Open group related to image processing research resources
- An introduction to some of the more exciting recent advances and dynamic current areas of development in biomedical Raman spectroscopy (including video-rate biomedical imaging). Illuminating disease and enlightening biomedicine: Raman spectroscopy as a diagnostic tool. http://pubs.rsc.org/en/content/articlepdf/2013/AN/C3AN00698K Analyst, 2013,138, 3871–3884
- Medical Imaging Explained Understanding the types and principles of medical imaging will support knowledge about a variety of machines and techniques about diagnostic imaging.
- Biomedical Imaging and Signal Analysis
- Henry Stewart Talks Series on Medical Imaging Imaging Techniques for Pre-clinical and Clinical Applications
