Cabergoline
 | |
| Clinical data | |
|---|---|
| Trade names | Cabaser, Dostinex |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category |
|
| Routes of administration | Oral |
| ATC code | G02CB03 (WHO) N04BC06 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | First-pass effect seen; absolute bioavailability unknown |
| Protein binding | Moderately bound (40–42%); concentration-independent |
| Metabolism | Hepatic, predominately via hydrolysis of the acylurea bond or the urea moiety |
| Biological half-life | 63–69 hours (estimated) |
| Excretion | Urine (22%), feces (60%) |
| Identifiers | |
| |
| CAS Number |
81409-90-7 |
| PubChem (CID) | 54746 |
| IUPHAR/BPS | 37 |
| DrugBank |
DB00248 |
| ChemSpider |
49452 |
| UNII |
LL60K9J05T |
| KEGG |
D00987 |
| ChEBI |
CHEBI:3286 |
| ChEMBL |
CHEMBL1201087 |
| Chemical and physical data | |
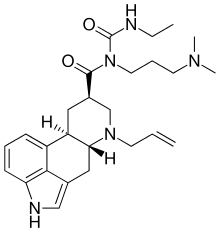
| Formula | C26H37N5O2 |
| Molar mass | 451.604 g/mol |
| 3D model (Jmol) | Interactive image |
| |
| |
| | |
Cabergoline (brand names Caberlin, Dostinex and Cabaser), an ergot derivative, is a potent dopamine receptor agonist on D2 receptors. Rat studies show cabergoline has a direct inhibitory effect on pituitary lactotroph (prolactin) cells.[1] It is frequently used as a first-line agent in the management of prolactinomas due to its higher affinity for D2 receptor sites, less severe side effects, and more convenient dosing schedule than the older bromocriptine.
Uses
- hyperprolactinemia[2]
- adjunctive therapy of prolactin-producing pituitary gland tumors (prolactinomas);
- monotherapy of Parkinson's disease in the early phase;
- combination therapy, together with levodopa and a decarboxylase inhibitor such as carbidopa, in progressive-phase Parkinson's disease;
- in some countries also: ablactation and dysfunctions associated with hyperprolactinemia (amenorrhea, oligomenorrhea, anovulation, nonpuerperal mastitis and galactorrhea);
- treatment of uterine fibroids.[3][4]
- adjunctive therapy of acromegaly, cabergoline has low efficacy in suppressing growth hormone levels and is highly efficient in suppressing hyperprolactinemia that is present in 20-30% of acromegaly cases; growth hormone and prolactin are similar structurally and have similar effects in many target tissues, therefore targeting prolactin may help symptoms when growth hormone secretion can not be sufficiently controlled by other methods;
Off-label
It has at times been used as an adjunct to SSRI antidepressants as there is some evidence that it counteracts certain side effects of those drugs, such as reduced libido and anorgasmia. It also has been suggested online that it has a possible recreational use in reducing or eliminating the male refractory period, thereby allowing men to experience multiple ejaculatory orgasms in rapid succession, and at least one scientific study supports those speculations.[5] It is also used by bodybuilders to control gynecomastia caused by elevated prolactin levels through the use of anabolic steroids such as nandrolone. Additionally, a systematic review and meta-analysis concluded that prophylactic treatment with cabergoline reduces the incidence, but not the severity, of ovarian hyperstimulation syndrome (OHSS), without compromising pregnancy outcomes, in females undergoing stimulated cycles of in vitro fertilization (IVF).[6] Also, a study on rats found that cabergoline reduces voluntary alcohol consumption, possibly by increasing GDNF expression in the ventral tegmental area.[7]
Contraindications and precautions
- Hypersensitivity to ergot derivatives
- Pediatric patients (no clinical experience)
- Severely impaired liver function or cholestasis
- Co-medication with drugs metabolized mainly by CYP P450 such as erythromycin and ketoconazole, because increased plasma levels of cabergoline may result (although cabergoline undergoes minimal CYP450 metabolism).
- Cautions: severe cardiovascular disease, Raynaud's disease, gastroduodenal ulcers, active gastrointestinal bleeding, hypotension.
Pregnancy and lactation
Relatively little is known about the effects of this medication during pregnancy and lactation. In some cases the related bromocriptine may be an alternative when pregnancy is expected.
- Pregnancy: available preliminary data indicates a somewhat increased rate of congenital abnormalities in patients who became pregnant while treated with cabergoline.. However, one study concluded that "foetal exposure to cabergoline through early pregnancy does not induce any increase in the risk of miscarriage or foetal malformation." [8]
- Lactation: In rats cabergoline was found in the maternal milk. Since it is not known if this effect also occurs in humans, breastfeeding is usually not recommended if/when treatment with cabergoline is necessary.
- Lactation suppression: In some countries cabergoline (Dostinex) is sometimes used as a lactation suppressant. It is also used in veterinary medicine to treat false pregnancy in dogs.
Side effects
Side effects are mostly dose dependent. Much more severe side effects are reported for treatment of Parkinson's disease and (off-label treatment) for restless leg syndrome which both typically require very high doses. The side effects are considered mild when used for treatment of hyperprolactinemia and other endocrine disorders or gynecologic indications where the typical dose is 10–100 times smaller than for Parkinson's disease.
Cabergoline requires slow dose titration (2–4 weeks for hyperprolactinemia, often much longer for other conditions) to minimise side effects. The extremely long bioavailability of the medication may complicate dosing regimens during titration and require particular precautions.
Cabergoline is considered the best tolerable option for hyperprolactinemia treatment although the newer and less tested quinagolide may offer similarly favourable side effect profile with quicker titration times.
Approximately 200 patients with newly diagnosed Parkinson's disease participated in a clinical study of cabergoline monotherapy. Seventy-nine (79) percent reported at least one side effect. These side effects were chiefly mild or moderate:
- GI tract: Side effects were extremely frequent. Fifty-three percent of patients reported side effects. Very frequent: Nausea (30%), constipation (22%), and dry mouth (10%). Frequent: Gastric irritation (7%), vomiting (5%), and dyspepsia (2%).
- Psychiatric disturbances and central nervous system (CNS): Altogether 51 percent of patients were affected. Very frequent: Sleep disturbances (somnolence 18%, insomnia 11%), vertigo (27%), and depression (13%). Frequent: dyskinesia (4%) and hallucinations (4%).
- Cardiovascular: Approximately 30 percent of patients experienced side effects. Most frequent were hypotension (10%), peripheral edema (14%) and non-specific edema (2%). Arrhythmias were encountered in 4.8%, palpitations in 4.3%, and angina pectoris in 1.4%.
In a combination study with 2,000 patients also treated with levodopa, the incidence and severity of side effects was comparable to monotherapy. Encountered side effects required a termination of cabergoline treatment in 15% of patients. Additional side effects were infrequent cases of hematological side effects, and an occasional increase in liver enzymes or serum creatinine without signs or symptoms.
As with other ergot derivatives, pleuritis, exudative pleura disease, pleura fibrosis, lung fibrosis, and pericarditis are seen. These side effects are noted in less than 2% of patients. They require immediate termination of treatment. Clinical improvement and normalization of X-ray findings are normally seen soon after cabergoline withdrawal. It appears that the dose typically used for treatment of hyperprolactinemia is too low to cause this type of side effects.
Valvular heart disease
In two studies published in the New England Journal of Medicine on January 4, 2007, cabergoline was implicated along with pergolide in causing valvular heart disease.[9][10] As a result of this, the FDA removed pergolide from the U.S. market on March 29, 2007.[11] Since cabergoline is not approved in the U.S. for Parkinson's Disease, but for hyperprolactinemia, the drug remains on the market. The lower doses required for treatment of hyperprolactinemia have been found to be not associated with clinically significant valvular heart disease or cardiac valve regurgitation.[12][13]
Interactions
No interactions were noted with levodopa or selegiline. The drug should not be combined with other ergot derivatives. Dopamine antagonists such as antipsychotics and metoclopramide counteract some effects of cabergoline. The use of antihypertensive drugs should be intensively monitored because excessive hypotension may result from the combination.
Pharmacology
Although cabergoline is commonly described principally as a dopamine D2 receptor agonist, it also possesses significant affinity for the D3, D4, 5-HT1A, 5-HT2A, 5-HT2B, 5-HT2C, α2B- receptors, and moderate/low affinity for the D1 and 5-HT7 receptors. Cabergoline functions as an agonist at all of these receptors except for 5-HT7 and α2B-, where it acts as an antagonist.[14]
Binding profile[15]
| Receptor | Binding Affinity (Ki [nM]) | Action |
|---|---|---|
| 5-HT1A | 20.0 | Agonist |
| 5-HT1B | 479 | Unknown |
| 5-HT1D | 8.71 | Unknown |
| 5-HT2A | 6.17 | Agonist |
| 5-HT2B | 1.17 | Agonist |
| 5-HT2C | 692 | Agonist |
| α1A adrenergic | 288 | Unknown |
| α1B adrenergic | 60.3 | Unknown |
| α1D adrenergic | 166 | Unknown |
| α2A adrenergic | 12 | Unknown |
| α2B adrenergic | 72.4 | Antagonist |
| α2C adrenergic | 22.4 | Unknown |
| β1 adrenergic | >10,000 | Unknown |
| β2 adrenergic | >10,000 | Unknown |
| D1 | 214 | Agonist |
| D2S | 0.62 | Agonist |
| D2L | 0.95 | Agonist |
| D3 | 0.79 | Agonist |
| D4 | 56.2 | Agonist |
| D5 | 22.4 | Unknown |
Pharmacokinetics
Following a single oral dose, resorption of cabergoline from the gastrointestinal (GI) tract is highly variable, typically occurring within 0.5 to 4 hours. Ingestion with food does not alter its absorption rate. Human bioavailability has not been determined since the drug is intended for oral use only. In mice and rats the absolute bioavailability has been determined to be 30 and 63 percent, respectively. Cabergoline is rapidly and extensively metabolized in the liver and excreted in bile and to a lesser extent in urine. All metabolites are less active than the parental drug or inactive altogether. The human elimination half-life is estimated to be 63 to 68 hours in patients with Parkinson's disease and 79 to 115 hours in patients with pituitary tumors. Average elimination half-life is 80 hours.
The therapeutic effect in treatment of hyperprolactinemia will typically persist for at least 4 weeks after cessation of treatment.
Mechanism of action
Cabergoline is a long-acting dopamine D2 receptor agonist and in vitro rat studies show a direct inhibitory effect on the prolactin secretion in the pituitary's lactotroph cells. Cabergoline decreased serum prolactin levels in reserpinized rats.
Receptor binding studies indicate a low affinity for dopamine D1 receptors, α1-adrenergic receptors, and α2-adrenergic receptors.[1]
Research
Cabergoline was studied in one person with Cushing's disease, to lower ACTH levels and cause regression of ACTH producing pituitary adenomas.[16]
History
Cabergoline was first synthesized by scientists working for the Italian drug company Farmitalia-Carlo Erba in Milan who were experimenting with semisynthetic derivatives of the ergot alkaloids, and a patent application was filed in 1980.[17][18][19] The first publication was a scientific abstract at the Society for Neuroscience meeting in 1991.[20][21]
Farmitalia-Carlo Erba was acquired by Pharmacia in 1993,[22] which in turn was acquired by Pfizer in 2003.[23]
Cabergoline was first marketed in The Netherlands as Dostinex in 1992.[17] The drug was approved by the FDA on December 23, 1996.[24] It went generic in late 2005 following US patent expiration.[25]
See also
References
- 1 2 "Dostinex at www.rxlist.com". Retrieved 2007-04-27.
- ↑ UK electronic Medicines Compendium Dostinex Tablets Last Updated on eMC Dec 23, 2013
- ↑ Sayyah-Melli, M; Tehrani-Gadim, S; Dastranj-Tabrizi, A; Gatrehsamani, F; Morteza, G; Ouladesahebmadarek, E; Farzadi, L; Kazemi-Shishvan, M (2009). "Comparison of the effect of gonadotropin-releasing hormone agonist and dopamine receptor agonist on uterine myoma growth. Histologic, sonographic, and intra-operative changes". Saudi medical journal. 30 (8): 1024–33. PMID 19668882.
- ↑ Sankaran, S.; Manyonda, I. (2008). "Medical management of fibroids". Best Practice & Research Clinical Obstetrics & Gynaecology. 22 (4): 655–76. doi:10.1016/j.bpobgyn.2008.03.001. PMID 18468953. http://www.britishfibroidtrust.org.uk/journals/bft_Sankaran.pdf
- ↑ Krüger TH, Haake P, Haverkamp J, et al. (December 2003). "Effects of acute prolactin manipulation on sexual drive and function in males". Journal of Endocrinology. 179 (3): 357–65. doi:10.1677/joe.0.1790357. PMID 14656205.
- ↑ Youssef MA, van Wely M, Hassan MA, et al. (March 2010). "Can dopamine agonists reduce the incidence and severity of OHSS in IVF/ICSI treatment cycles? A systematic review and meta-analysis". Hum Reprod Update. 16 (5): 459–66. doi:10.1093/humupd/dmq006. PMID 20354100.
- ↑ Carnicella, S.; Ahmadiantehrani, S.; He, D. Y.; Nielsen, C. K.; Bartlett, S. E.; Janak, P. H.; Ron, D. (2009). "Cabergoline Decreases Alcohol Drinking and Seeking Behaviors Via Glial Cell Line-Derived Neurotrophic Factor". Biological Psychiatry. 66 (2): 146–153. doi:10.1016/j.biopsych.2008.12.022. PMC 2895406
 . PMID 19232578.
. PMID 19232578. - ↑ Colao, A; Abs R.; et al. (January 2008). "Pregnancy outcomes following cabergoline treatment: extended results from a 12-year observational study". Clinical Endocrinology. 68 (1): 66–71. doi:10.1111/j.1365-2265.2007.03000.x. PMID 17760883.
- ↑ Schade, Rene; Andersohn, Frank; Suissa, Samy; Haverkamp, Wilhelm; Garbe, Edeltraut (2007-01-04). "Dopamine Agonists and the Risk of Cardiac-Valve Regurgitation". New England Journal of Medicine. 356 (1): 29–38. doi:10.1056/NEJMoa062222. PMID 17202453.
- ↑ Zanettini, Renzo; Antonini, Angelo; Gatto, Gemma; Gentile, Rosa; Tesei, Silvana; Pezzoli, Gianna (2007-01-04). "Valvular Heart Disease and the Use of Dopamine Agonists for Parkinson's Disease". New England Journal of Medicine. 356 (1): 39–46. doi:10.1056/NEJMoa054830. PMID 17202454.
- ↑ "Food and Drug Administration Public Health Advisory". 2007-03-29. Archived from the original on 2007-04-08. Retrieved 2007-04-27.
- ↑ Bogazzi, F.; Buralli, S.; Manetti, L.; Raffaelli, V.; Cigni, T.; Lombardi, M.; Boresi, F.; Taddei, S.; Salvetti, A. (2008). "Treatment with low doses of cabergoline is not associated with increased prevalence of cardiac valve regurgitation in patients with hyperprolactinaemia". International Journal of Clinical Practice. 62 (12): 1864–9. doi:10.1111/j.1742-1241.2008.01779.x. PMID 18462372.
- ↑ Wakil, A.; Rigby, A. S; Clark, A. L; Kallvikbacka-Bennett, A.; Atkin, S. L (2008). "Low dose cabergoline for hyperprolactinaemia is not associated with clinically significant valvular heart disease". European Journal of Endocrinology. 159 (4): R11–4. doi:10.1530/EJE-08-0365. PMID 18625690.
- ↑ Sharif NA, McLaughlin MA, Kelly CR, Katoli P, Drace C, Husain S, Crosson C, Toris C, Zhan GL, Camras C (March 2009). "Cabergoline: Pharmacology, ocular hypotensive studies in multiple species, and aqueous humor dynamic modulation in the Cynomolgus monkey eyes". Experimental Eye Research. 88 (3): 386–97. doi:10.1016/j.exer.2008.10.003. PMID 18992242.
- ↑ National Institute of Mental Health. PDSD Ki Database (Internet) [cited 2013 Jul 24]. ChapelHill (NC): University of North Carolina. 1998-2013. Available from: "Archived copy". Archived from the original on 2013-11-08. Retrieved 2014-03-04.
- ↑ Miyoshi, T.; et al. (2004). "Effect of cabergoline treatment on Cushing's disease caused by aberrant adrenocorticotropin-secreting macroadenoma". Journal of endocrinological investigation. 27 (11): 1055–1059. doi:10.1007/bf03345309. PMID 15754738.
- 1 2 Council regulation (EEC) no 1768/92 in the matter of Application No SPC/GB94/012 for a Supplementary Protection Certificate in the name of Farmitalia Carlo Erba S. r. l.
- ↑ Espace record: GB 202074566
- ↑ US Patent 4526892 - Dimethylaminoalkyl-3-(ergoline-8'.beta.carbonyl)-ureas
- ↑ Fariello, RG (1998). "Pharmacodynamic and pharmacokinetic features of cabergoline. Rationale for use in Parkinson's disease". Drugs. 55 (Suppl 1): 10–6. PMID 9483165.
- ↑ Carfagna N, Caccia C, Buonamici M, Cervini MA, Cavanus S, Fornaretto MG, Damiani D, Fariello RG (1991). "Biochemical and pharmacological studies on cabergoline, a new putative antiparkinsonian drug". Soc Neurosci Abs. 17: 1075.
- ↑ Staff. News: Farmitalia bought by Kabi Pharmacia. Ann Oncol (1993) 4 (5): 345.
- ↑ Staff, CNN/Money. April 16, 2003 It's official: Pfizer buys Pharmacia
- ↑ FDA approval history
- ↑ FDA generic approvals, December 2005